Primary motor cortex damage often causes problems with movement and coordination. Fortunately, many individuals with impaired motor control due to primary motor cortex damage can improve their mobility and quality of life.
To help you overcome primary motor cortex damage, this article will discuss:
Primary Motor Cortex Functions
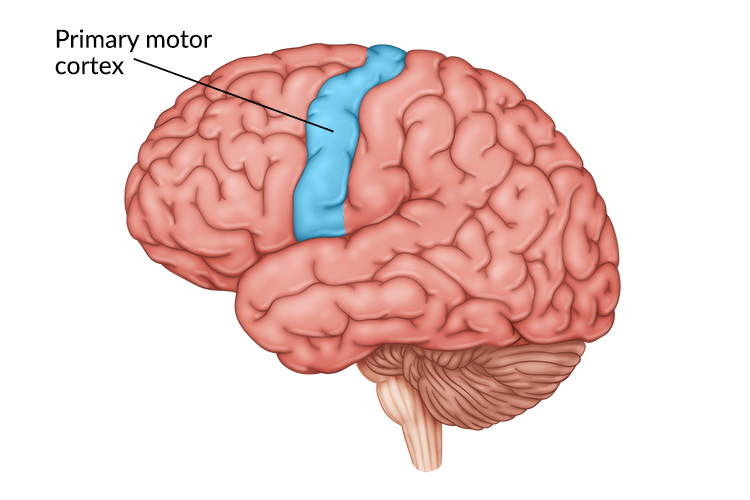
The primary motor cortex is a strip of brain tissue located in the frontal lobe. It is responsible for initiating purposeful and intentional movements. These purposeful movements include everything from moving your hands, arms, and legs to controlling facial expressions and even swallowing.
In a normal functioning primary motor cortex, signals cross over the center of the body to activate muscles on the opposite side. This means that the movements on the right side of your body are controlled by the left hemisphere of the primary motor cortex, and vice versa.
Additionally, different areas of the primary motor cortex control different parts of the body. While every body part is represented in the primary motor cortex, not every part has equal amounts of brain matter devoted to it.
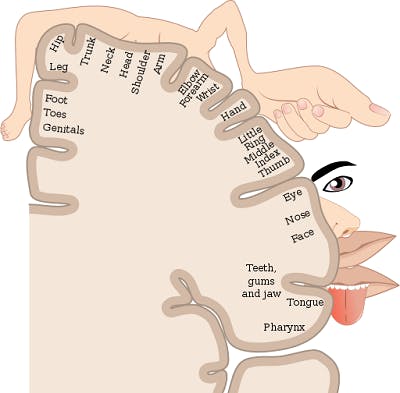
For example, complex movements that require precise control take up larger amounts of space in the brain than simple motions do. A significant portion of the motor cortex is devoted to finger movements and facial expressions, while a smaller portion of the brain is responsible for leg motions.
This explains why many individuals struggle with fine motor control or facial paralysis after brain injury. Because those movements are controlled by a larger portion of the motor cortex, they have a much higher likelihood of becoming damaged during an injury.
To help you understand what happens when the motor cortex is damaged, the following section will discuss potential secondary effects.
Want 25 pages of TBI recovery exercises in PDF form? Click here to download our free TBI Rehab Exercise ebook now (link opens a pop up for uninterrupted reading)
What Happens if the Motor Cortex is Damaged?
Besides causing general problems with movement, there are some specific signs that indicate damage to the primary motor cortex. These are known collectively as upper motor neuron syndrome.
There are five main signs of upper motor neuron syndrome, which we will examine below.
1. Hemiparesis
This refers to weakness on one side of the body. It is most common in stroke survivors but can also occur after other neurological conditions, too.
If damage occurs in the left motor cortex, an individual’s right side will be weakened significantly. They may have trouble lifting their right arm, moving the fingers on their right hand, and the entire right side of their face might droop.
2. Overactive Reflexes
Deep tendon reflexes, also known as ‘muscle stretch reflexes,’ are the involuntary reactions of a muscle when stretched by its neighboring tendon. These reflexes are often overactive (exaggerated) in individuals with upper motor neuron syndrome and can present as clonus or spasticity.
There are different types of overactive reflexes, including:
- Clonus occurs when the electrical signals sent by the brain to the muscles are interrupted. This can happen after direct damage to the motor cortex or damage along any of the descending motor pathways. It creates repetitive and rapid involuntary muscle contractions that often occur in a rhythmic pattern.
- Spasticity is characterized by prolonged, involuntary muscle contractions. If spasticity goes unmanaged, the muscle fibers can shorten and contracture may set in.
- Babinski sign refers to an abnormal reflex that causes the big toe to move upwards and the rest of the toes to fan out when the bottom of the foot is stroked.
3. Decreased Motor Control
When an injury damages the primary motor cortex, the person will typically experience a loss of coordination and poor dexterity. For example, the person usually loses the ability to perform fine motor movements that involve the muscles of the hands, fingers, and wrists.
The ability to move each individually and coordinate movements is known as fine motor skills. Some examples of activities that require fine motor skills include:
- Fastening buttons on a shirt
- Brushing teeth or shaving
- Writing or typing
- Playing musical instruments or video games
After a brain injury, these skills can become more difficult, if not impossible, to perform.
4. Altered Muscle Tone
Upper motor neuron syndrome typically involves a change in the individual’s muscle tone, whether that is hypotonia (low/decreased muscle tone) or hypertonia (high/increased muscle tone). Both conditions can affect mobility and coordination.
5. Decreased Endurance
The muscles of an individual who has sustained damage to the primary motor cortex typically fatigue very easily. As a result, individuals may experience decreased endurance when performing activities or tasks.
Fortunately, upper motor neuron syndrome can often be improved after brain damage by promoting the brain’s ability to make adaptive changes.
Treatment for Primary Motor Cortex Damage

While it’s not possible to repair primary motor cortex damage, it is possible to regain lost functions.
The brain possesses a remarkable healing ability to make adaptive changes known as neuroplasticity. It allows for functions affected by damage to be reorganized to unaffected regions of the brain and strengthened through repetitive practice.
Below, we’ll discuss several treatments that may be involved in recovering functions after primary motor cortex damage.
Physical Therapy
One of the most effective ways to recover motor control after primary motor cortex damage is to participate in physical therapy.
Physical therapy improves mobility by focusing on the repetitive practice of targeted exercises. By targeting the affected muscle groups, individuals can stimulate the brain and reinforce demand for those functions. This will encourage the brain to utilize neuroplasticity to rewire and strengthen the neural pathways for those functions.
Occupational Therapy
Occupational therapy can help individuals with primary motor cortex damage develop their independence. This typically involves practicing activities of daily living such as dressing, grooming, and feeding.
By consistently practicing these activities or learning new ways to compensate for limited movement, individuals can improve their functional abilities.
Speech Therapy
Individuals who experience weakness or paralysis in the facial muscles after primary motor cortex damage may benefit from participating in speech therapy.
Orofacial motor impairments can affect an individual’s breathing, chewing, swallowing, and speaking. By participating in speech therapy, individuals can practice activities and exercises to strengthen their oral motor muscles and improve overall communication skills.
Orthotics
Individuals who develop abnormal muscle tone or overactive reflexes after primary motor cortex damage may be recommended orthotics such as braces and splints. Orthotics provide musculoskeletal support and help ensure that the body part is correctly aligned.
Often, high muscle tone can pull the body into abnormal postures and affect an individual’s resting position and movement. Orthotics can help hold the affected limbs in place and reduce the extent of further muscle tightening.
Muscle Relaxants/ Botox Injections
High muscle tone can significantly limit a person’s range of motion. To relax the muscles, individuals with primary motor cortex damage may be recommended muscle relaxants such as baclofen or nerve blockers such as Botox.
Depending on how much of the body is affected, various forms of relief may be recommended. For example, oral muscle relaxants affect the entire body while injections allow for more localized relief.
It’s also important to understand that these medications only provide temporary relief. Therefore, it is recommended that individuals take advantage of the reduced muscle tone to participate in therapeutic exercises and activities to sustain more long-term relief.
Home Exercise
To ensure that you recover from primary motor cortex damage, it’s crucial to do your therapy exercises as often as you can. One hour, three times a week is usually the most you can get from a rehab clinic, but continuing your therapy at home between sessions will help you to make real progress.
That’s why home therapy devices such as FitMi or MusicGlove are so helpful. They motivate patients to perform hundreds of exercises at home, all in a fun and engaging way.
This is critical because the more exercises you do, the faster you will recover function.
Primary Motor Cortex Damage: Key Points
Primary motor cortex damage can affect voluntary motor control throughout the entire body. Fortunately, many individuals can improve their mobility by participating in rehabilitative therapies and other interventions that focus on promoting neuroplasticity.
With enough practice, individuals may be able to gradually improve their mobility and significantly improve their quality of life.