Spinal cord injury can affect many bodily functions and processes, including processes that are autonomic, or involuntary. This includes things such as breathing, blood pressure regulation, and digestion. The vagus nerve plays a valuable role in these processes by relaying information between the organs and the nervous system.
After spinal cord injury, these processes can be affected due to damage to the nervous system. However, stimulation of the vagus nerve may be an effective treatment during spinal cord injury recovery to help regulate these bodily functions.
In this article we will discuss how the vagus nerve functions as well as how spinal cord injury affects the vagus nerve. We will also explore the use of vagus nerve stimulation as a spinal cord injury treatment.
What is the Vagus Nerve?
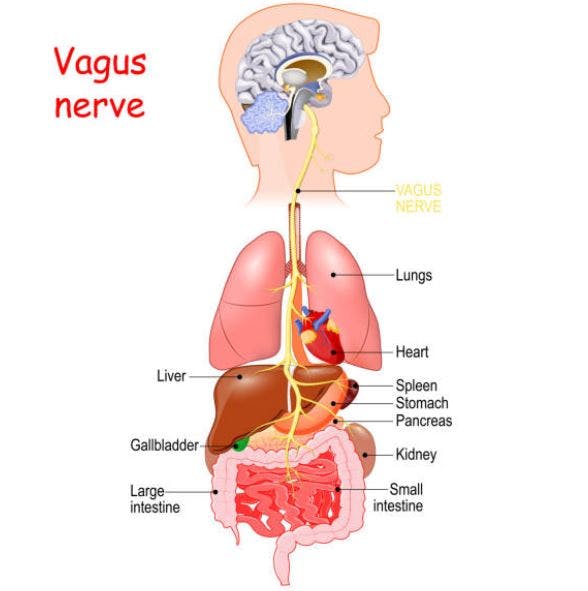
The vagus nerve is the tenth cranial nerve and is the largest of the twelve pairs of cranial nerves that stem from the brain. “Vagus” means wanderer in Latin, which perfectly embodies the way the nerve affects many organs and a wide range of essential body functions.
Primary functions of the vagus nerve include:
- Decreasing heart rate and blood pressure
- Regulating respiration (breathing rate)
- Stimulating digestion
- Decreasing inflammation
- Reducing depression and anxiety
The vagus nerve branches off the brainstem in many different directions and innervates numerous body structures. This includes the throat, larynx (voice box), heart, tongue, external ears, lungs, and gastrointestinal tract. Due to this widespread distribution, the vagus nerve plays a significant role in regulating your parasympathetic nervous system. This system is responsible for your “rest and digest” or relaxation functions.
When the vagus nerve is stimulated, its tone increases. High vagal tone allows you to relax by decreasing alertness, slowing down your heart rate, speeding up digestion, and relaxing your bladder and bowel muscles.
What Happens to the Vagus Nerve After Spinal Cord Injury?
The vagus nerve is not directly affected by spinal cord injury because it is not part of the spinal column. The cranial nerves are located above the spinal cord and branch out separately from different areas of the brain. However, many organs and muscles are dually innervated by sensory neurons from the spinal cord and vagus nerve.
Throughout the day, your body switches off between a state of “rest and digest” (parasympathetic response) and “fight or flight” (sympathetic response). These systems prepare your body for more intense periods of activity or arousal and, alternatively, allow the body to return to a relaxed state known as homeostasis.
After a spinal cord injury (typically at level T6 and higher), people are at risk for experiencing autonomic dysreflexia. This occurs when the body overreacts after encountering noxious, or harmful, stimuli to areas below the level of injury.
When the body detects noxious stimuli, the “fight or flight” response is activated, causing a spike in blood pressure, sweating, respiration, and anxiety. In individuals without spinal cord injury, the message about the noxious stimuli would be sent to the brain and the brain would send a signal back to the body telling it to move away from the stimuli. In turn, this would allow the parasympathetic system to take over and help return the body to a state of relaxation.
After a spinal cord injury, this communication pathway is disrupted and the brain may be unable to relay these messages to the appropriate nerves. This prevents the vagus nerve from intervening and inhibits the typical relaxation response. This means the body is unable to return to a restful state (where blood pressure comes back down, etc.) until the noxious stimulus is removed or resolved.
Can Vagus Nerve Stimulation Promote Spinal Cord Injury Recovery?
There is growing evidence to support vagus nerve stimulation as a spinal cord injury intervention. Vagus nerve stimulation (VNS) is administered through a biomedical device that is surgically implanted under the skin. This device transmits mild electrical currents through the vagus nerve, which then travel to the brain.
While it won’t treat your spinal cord injury directly, vagus nerve stimulation can potentially help regulate the autonomic nervous system to maintain homeostasis. By lowering heart rate, blood pressure, inflammation, and respiration rate, vagus nerve stimulation can reduce stress, anxiety, and depression. Additionally, it increases the release of neurotransmitters like norepinephrine, serotonin, and dopamine to improve motivation, mood, and reward perception.
While research on the effectiveness of vagus nerve stimulation for spinal cord injury in humans is still somewhat limited, animal studies have found that VNS can help decrease neuroinflammation. When the vagus nerve is stimulated, this can inhibit pro-inflammatory factors and increase release of anti-inflammatory factors. This helps to boost healing after spinal cord injury and can enhance recovery of motor function.
Additionally, vagus nerve stimulation is an FDA-approved treatment for depression, which is a secondary effect commonly experienced after spinal cord injury. Vagus nerve stimulation can improve your mental and physical health so your body is in the best condition to pursue recovery.
It is important to note that research has shown vagus nerve stimulation to be more effective when paired with rehabilitation therapy. This maximizes neuroplasticity, the brain’s ability to heal and make new connections. Talk with your physical and/or occupational therapist about what rehab plan and exercises are optimal for your recovery journey.
Side Effects of Vagus Nerve Stimulation
Since the vagus nerve affects many bodily functions, stimulation of this nerve can be accompanied by many potential side effects. These side effects are most often present in the early stages of vagus nerve stimulation and generally diminish with time.
Side effects of vagus nerve stimulation can include:
- Voice changes or hoarseness
- Sore throat or difficulty swallowing
- Shortness of breath
- Coughing
- Headache or dizziness
- Stomach upset
If these symptoms are persistent following vagus nerve stimulation, it is important to speak to your doctor as the stimulation may need to be reduced. Furthermore, it is necessary to inform your healthcare provider about your VNS implant before undergoing imaging such as MRI.
The Importance of the Vagus Nerve After Spinal Cord Injury
The vagus nerve helps regulate the autonomic nervous system, which allows the body to maintain homeostasis. This nerve is crucial after a spinal cord injury as it can play a role in regulating autonomic dysreflexia as well as involuntary bodily functions such as blood pressure, respiration, and digestion.
Vagus nerve stimulation can help address and improve mental and physical health, which helps keep secondary effects like depression in check. Additionally, vagus nerve stimulation can include benefits such as decreased neuroinflammation, improved autonomic function, and enhanced motor performance. Vagus nerve stimulation after spinal cord injury is also more effective when accompanied by rehabilitation therapy.
Health is multifactorial and, by adjusting physical factors like heart rate, blood pressure, and digestion, spinal cord injury patients can feel more relaxed and motivated to pursue recovery. We hope this article has helped explain the role of the vagus nerve after spinal cord injury as well as the potential benefits of vagus nerve stimulation.