Nystagmus refers to a secondary effect of head injury that causes the eyes to make rapid, uncontrolled movements. It usually occurs after cerebellar damage. Vestibular disorders can also sometimes cause nystagmus.
This article will help you understand the causes and signs of nystagmus after a head injury. We’ll also cover some exercises that can reduce nystagmus if it is caused by inner ear problems.
Causes of Nystagmus After Head Injury
Nystagmus, also known as “dancing eyes,” causes involuntary, rapid eye movements in one or both eyes.
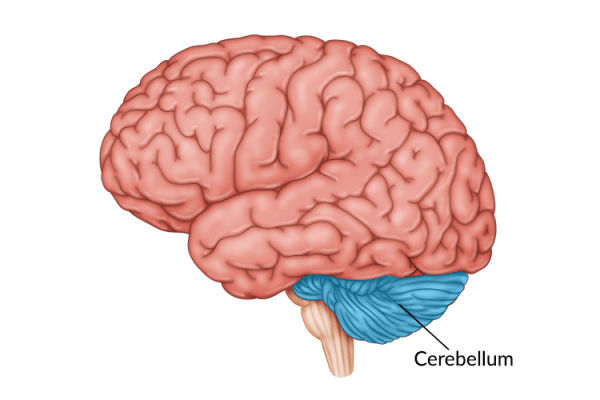
It occurs when the part of the brain that controls eye positioning does not function correctly. Although there are several areas of the brain that control eye movement, nystagmus is most often associated with damage to the cerebellum or brainstem.
Damage to the inner ear can also lead to nystagmus. The inner ear is part of the vestibular system, which helps the body maintain its balance. Part of staying balanced involves keeping eye movements steady and smooth.
When the inner ear is affected after a head injury, the brain can no longer tell what position the head is in. When this delicate system is damaged, the brain does not know which position the eyes must be in. As a result, the eyes will bounce around in a seemingly random fashion.
Signs of Nystagmus after Head Injury
Signs of nystagmus mainly include fast, uncontrollable eye movements. The direction of the eye movement can look a little different in each person though. In fact, there are three main types of movement a person with nystagmus can experience after head injury:
- Horizontal nystagmus which involves side-to-side eye movements.
- Vertical nystagmus which causes up and down movements.
- Rotary nystagmus which involves circular eye movements.
These movements can occur in one or both eyes.
Nystagmus can affect eyesight and cause varying degrees of dizziness, though for most people their vision is not severely affected.
Treatments for Nystagmus

Some mild forms of nystagmus after a head injury can be treated with corrective lenses or contacts. In more severe cases, certain drugs like Baclofen can help reduce nystagmus movements.
Most of these treatments are only temporary, however, and do not address the root causes of nystagmus. Therefore, the best way to eliminate nystagmus is to treat whatever underlying issues that may be triggering it.
A vestibular specialist can help you determine whether your nystagmus is caused by inner ear problems or brain damage. If inner ear damage is causing your nystagmus, vestibular therapy might help.
The following are a few exercises that may help improve your sense of balance and improve nystagmus after a head injury:
1. Epley Maneuver
A head injury can cause the crystals in your inner ear to dislodge, which can lead to severe vertigo and a condition called Benign Paroxysmal Positional Vertigo (BPPV). The Epley maneuver was designed to move those crystals back into their proper place.
It involves moving the head into four positions and staying in each position for about thirty seconds.
The Epley maneuver must be performed by a vestibular specialist and should never be performed on your own. You can find a list of certified vestibular specialists here.
2. Gaze Stabilization Exercises

The link between the inner ear and eye movement is seen most clearly in the vestibulo-ocular reflex. This is what allows your eyes to stay focused on an object while your head is moving.
After a head injury, this reflex can become damaged, which will cause disorientation, loss of focus, vertigo, and in some cases, nystagmus.
Gaze stabilization exercises were designed to help restore the vestibulo-ocular reflex, which can help reduce nystagmus. It involves several exercises of increasing difficulty. The following is a sample exercise:
- Sit upright in a chair.
- Draw an X in the center of a piece of paper.
- Hold the paper at arm’s length. Keep it at eye level.
- While focusing on the X, turn your head side to side. Move as fast as you can without the X getting blurry.
- Do this for 1 minute or for as long as you can handle.
To see the most improvement, you will need to practice the exercises several times per day. That’s because the more you exercise, the more you will activate neuroplasticity, which will allow your brain to re-establish a connection to your vestibular system.
3. Brandt-Daroff Exercises
If you have been diagnosed with BPPV, you most likely will undergo treatments to put the crystals back into place. However, unlike the Epley maneuver, you can do the Brandt-Daroff exercises on your own, though we always recommend having a vestibular specialist help you.
Here’s how to perform the Brandt-Daroff exercises:
- Sit on the side of your bed.
- Lie down on your left side. As you are heading down, turn your head up at a 45-degree angle. Try to do both as quickly as possible.
- Remain on your side, with your head at a 45-degree angle, for 30 seconds.
- Sit up straight for thirty seconds.
- Repeat on your right side. Do five times on each side.
You’ll want to do these exercises at least twice a day until your symptoms improve.
While these exercises most likely will not completely cure your nystagmus, they can help treat inner ear problems, which might at least reduce the severity of your eye movements.
Once again though, talk to a vestibular specialist about your condition before trying any of these exercises.
Understanding Nystagmus After Head Injury
Nystagmus after a head injury can cause issues with vision, focus, balance, and varying degrees of dizziness. While some cases of nystagmus will resolve on their own, most will require some form of treatment.
A vestibular specialist is the best person to diagnose you and suggest the most appropriate treatment for your nystagmus. Some of the most common treatments include corrective lenses, baclofen injections, and vestibular therapy.
With the right treatment approach, you can have a real chance of regaining control over your eye movements and improving your vision after a head injury.
We hope this article has given you a better understanding of nystagmus after head injury.