After a spinal cord injury, you may experience clonus, which refers to involuntary rhythmic shaking of the limbs. If not properly managed, it can progress and significantly affect your mobility.
To help you better understand clonus after spinal cord injury, this article will go over its causes, symptoms, and management.
Causes of Clonus After Spinal Cord Injury
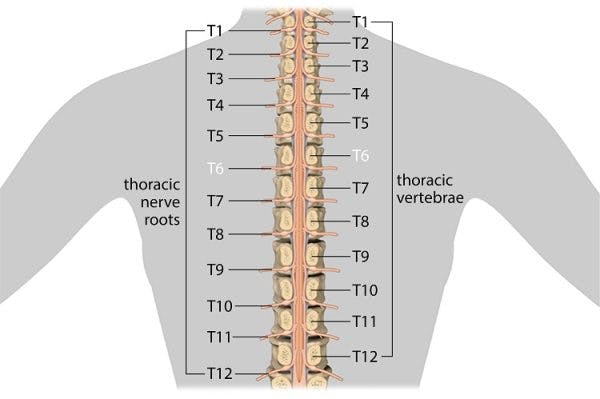
Clonus after spinal cord injury is a reflex caused by damage to the upper motor neurons. Upper motor neurons are nerve cells that originate in the brain and are responsible for relaying signals down the spinal cord to initiate movement in the muscles.
Because communication between the brain, spinal cord, and muscles is disrupted after SCI, reflexes often become hyperexcitable to stimulation. While the exact mechanisms underlying clonus have yet to be fully understood, it typically develops within 2 months after spinal cord injury.
Clonus is most common in the ankles and feet. However, depending on your level of injury, it can also occur in the knees, calves, wrists, triceps, and biceps.
Along with clonus, individuals with spinal cord injuries may also experience more sustained involuntary muscle contractions called spasticity. In the following section, we’ll discuss the difference between these two reflexes.
What is the Difference Between Spasticity and Clonus?

Spasticity and clonus are both outcomes of upper motor neuron damage characterized by involuntary muscle contractions. However, they describe two very different reactions.
Spasticity refers to velocity-dependent increases in muscle tone that create resistance to movement. The more rapidly a muscle is stretched, the more severely it contracts. Individuals with spasticity typically experience stiff movements due to prolonged involuntary muscle contractions.
In contrast, clonus describes uncontrollable jerking or rhythmic shaking of a limb due to fluctuations in the relaxing and contracting of muscles.
Clonus is also commonly mistaken for tremors. The main difference is that clonus is increased by muscle stretching, while tremors are often caused or exacerbated by stress, exhaustion, medication side effects, an overactive thyroid, intentional movements, or alcohol abuse.
Now that you have a better idea of what clonus is, we’ll discuss some ways to effectively manage it.
How to Manage Clonus After Spinal Cord Injury
The effects of every spinal cord injury are unique, so the severity of clonus varies from person to person. Some people may experience occasional, mild shaking while others may be unable to stand or walk.
Severe clonus can disrupt sleep, cause extreme fatigue, and make it difficult to perform self-care tasks.
To understand how to prevent clonus from progressing, we’ll discuss some of the most effective ways to manage it below.
1. Physical Therapy
Physical therapy for clonus management will primarily consist of stretching, range of motion, and strengthening exercises. Stretching helps lengthen tight muscles and repetitive exposure to movement may help reduce reflex excitability. Weight bearing exercises may also be used during physical therapy treatments.
The spinal cord is capable of rewiring itself by utilizing the central nervous system’s ability to make adaptive changes, known as neuroplasticity. The more you practice movements, the more your spinal cord recognizes a demand for that function, which helps promote circuit reorganization.
2. Cold Application
Another way to reduce the frequency and severity of clonus is through cold applications.
In this study, researchers wrapped crushed ice in wet towels around muscles prone to clonus for 10 minutes. Then, they had the participants exercise those muscle groups. The procedure resulted in immediate clonus reduction that lasted 12 hours.
Additionally, this study had participants partake in 10 sessions of both cryotherapy (cold therapy) and physical therapy. Compared to the control group (that only received physical therapy), individuals who participated in both cryotherapy and physical therapy experienced a significant decrease in clonus frequency.
If you’re considering using cold packs at home, be aware of the intensity and length of application. Oftentimes, sensation is affected by spinal cord injury, making it more likely that you could leave a cold pack on for too long, resulting in skin damage.
For individuals with sensation deficits, it is generally best to use a layer, such as a towel, between the cold pack and the skin, and to limit use to approximately 20 minutes or less, checking the skin occasionally.
3. Orthotics
Orthotic devices like braces, casts, and splints can also help individuals manage clonus after spinal cord injury. They provide additional structure and stability to mildly resist involuntary movements. Orthotics also gently lengthen tight muscles, which may help reduce hypersensitivity to movement and touch.
4. Botox
Because clonus generally affects a certain area of the body, Botox injections tend to be preferred over oral medications. Oral medications affect the entire body and have a greater risk of unwanted side effects like drowsiness and disorientation. In contrast, Botox is injected directly into the overactive muscle to provide localized clonus relief.
However, it’s important to understand that Botox will not treat clonus long-term because it does not address the central nervous system damage that causes it.
5. Surgery
Due to its invasive and costly nature, surgery is often used as a last resort when all other management interventions prove ineffective. Surgery for clonus involves incisions at the spinal nerves. This will cut off some innervation at those muscles, which will reduce their excitability.
Clonus and Spinal Cord Injury: Key Points
Clonus commonly occurs after spinal cord injuries due to upper motor neuron damage. The rhythmic shaking or jerking characteristic of clonus can interfere with your day-to-day life, so it’s essential to properly manage it to minimize its effects.
Hopefully, this article helped you better understand what clonus is, how it differs from spasticity, and how to effectively manage it.