Apraxia is a neurological disorder that interferes with the ability to properly execute a movement. This can make it challenging for an individual to perform activities of daily living as well as complex tasks that require sensory, motor, and coordination skills.
Apraxia is caused by damage to the areas of the brain responsible for movement and coordination. One of the most common types of apraxia after brain damage is buccofacial or orofacial apraxia, which affects the ability to execute mouth and facial movements or expressions. Fortunately, apraxia can often be improved through a rigorous rehabilitation program.
This article will discuss the causes of apraxia after brain damage, different types of apraxia, and treatments to help promote recovery.
Use the jump links below to navigate through the article:
What Causes Apraxia After Brain Damage?
Apraxia refers to the inability to execute coordinated movements despite having the desire and capacity. Even if sensory and motor functions are intact, individuals with apraxia may struggle to carry out purposeful movements. To understand why this occurs, it first helps to know how the brain and muscles work together to execute movement.
The primary structures of the brain associated with motor control and coordination include the cerebellum, basal ganglia, frontal lobe, prefrontal cortex, and parietal lobe. These structures all work together to send signals to the muscles, telling them when to contract and relax.
When these areas of the brain are affected by a neurological injury or disease, the brain may no longer be able to communicate efficiently with the appropriate muscles. This disruption in communication can lead to various movement disorders, including apraxia.
Neurological conditions that can cause apraxia after brain damage include:
- Traumatic brain injury
- Stroke
- Brain tumor
- Dementia
- Hydrocephalus (build-up of fluid in the cavities or ventricles deep in the brain)
- Other neurodegenerative diseases
Apraxia may also appear after birth if the brain sustained damage in the areas that control movement. Individuals who experience brain damage due to any of these conditions may lose the ability to properly execute movements and perform activities of daily living.
Fortunately, communication between the brain and muscles can be restored through neuroplasticity, the brain’s natural ability to rewire itself. Neuroplasticity works by strengthening neural connections and creating new ones, improving overall function.
Neuroplasticity is best activated through high repetition of rehabilitation exercises. The more a movement is practiced, the more the brain will learn to recognize that movement and strengthen its neural connections. The stronger the communication between the brain and the affected muscles, the higher the chances of executing a movement successfully.
Symptoms of Apraxia
Apraxia can affect many different muscle movements or functions, depending on the root cause. The different signs and symptoms individuals may experience depend on the type and severity of apraxia. A doctor or therapist can help individuals identify their exact type of apraxia and provide them with a unique treatment plan.
Generally, symptoms of apraxia can include:
- Lack of coordination
- Involuntary or unintentional movements
- Difficulty performing specific tasks
- Clumsy or inappropriate movements
- Difficulty reproducing patterns or drawings
- Trouble executing commands that were fully understood
More specific symptoms will depend on which type of apraxia an individual has. For example, survivors with limb-kinetic apraxia may have difficulty using their legs to walk or picking up objects with their arms.
Survivors with apraxia of speech (verbal apraxia) may experience delayed speech, exaggerated movements of the lips and tongue, distortion of vowel sounds, or difficulty stringing syllables together. Some may also struggle with omitting consonants at the beginning and/or end of words.
Since there are many speech disorders, it’s important to consult with a speech-language pathologist and obtain a proper diagnosis. With a proper apraxia diagnosis, individuals may begin treatment, which often includes a combination of therapies.
Types of Apraxia that Can Develop After Brain Damage
Several types of apraxia may occur after brain damage, depending on the structure(s) of the brain affected, such as the basal ganglia or prefrontal cortex. Many types of apraxia can occur simultaneously or sequentially, meaning individuals may experience more than one type of apraxia.
Some of the most common types of apraxia after brain damage include:
- Ideational apraxia makes it difficult for individuals to execute movements and perform tasks that involve multiple steps. This includes tasks such as dressing, eating, bathing, or other activities of daily living.
- Ideomotor apraxia causes difficulty following verbal commands to copy movements or follow suggestions for movements. Individuals with ideomotor apraxia can, however, perform automatic movements that they don’t have to think about or plan.
- Limb-kinetic apraxia refers to the inability to use a finger, arm, or leg to make fine, precise movements. For example, an individual may understand how to use a tool or utensil but may have difficulty carrying out that movement.
- Verbal apraxia, also known as apraxia of speech, causes difficulty with planning and coordinating the movements for speech. Individuals with verbal apraxia may know what they want to say but be unable to execute their words, leading to distorted words, rhythm, or inflection. Studies show that apraxia of speech may also be accompanied by aphasia, the inability to comprehend or produce language.
- Ocular motor apraxia is characterized by difficulty executing eye movements such as visually tracking or following a moving object.
- Buccofacial or orofacial apraxia inhibits the ability to perform mouth or facial movements on command, such as sticking out the tongue, whistling, winking, or even coughing.
- Conceptual apraxia can cause difficulty using objects appropriately. For example, when asked to demonstrate how to use a screwdriver, an individual with conceptual apraxia may use it as a hammer instead.
While apraxia affects the coordination and execution of muscle movements, different subtypes of apraxia may each present with unique symptoms. Fortunately, many symptoms of apraxia can be improved with a rigorous rehabilitation regimen and other treatments.
How to Treat Apraxia After Brain Damage
Treatment for apraxia after brain damage revolves around stimulating the brain and activating neuroplasticity (the brain’s ability to rewire itself) as much as possible. This will help restore communication between the brain and the affected muscles, which is necessary to improve coordination and movement quality.
Rehabilitation exercises will depend on the type of apraxia an individual has and the skills they want to improve. When survivors experience multiple types of apraxia disorders, such as apraxia of speech and limb-kinetic apraxia, therapists may recommend a combination of rehabilitation exercises to treat each condition separately.
Rehabilitation exercises for apraxia after brain damage may include:
- Physical therapy: typically focuses on improving mobility, strength, and coordination. Exercising the affected muscles can help activate neuroplasticity and restore communication between the brain and muscles. This type of therapy is particularly helpful for survivors with limb-kinetic or ideomotor apraxia.
- Occupational therapy: provides survivors with the tools they need to perform daily activities and helps them find compensatory tactics as they work toward recovery. Occupational therapy is particularly helpful for individuals with ideational apraxia or conceptual apraxia as these make it difficult to complete tasks that require more than one step.
- Speech therapy: focuses on improving speech and language disorders like apraxia of speech. Speech-Language Pathologists provide a unique therapy plan that includes a variety of speech exercises such as lip articulation, tongue articulation, and coordination exercises. They may also recommend facial strengthening exercises to individuals with buccofacial or orofacial apraxia.
The more an individual practices rehab exercises, the higher their chances of restoring neural communication and improving muscle function. Therefore, it’s important to keep the brain stimulated between therapy sessions to maximize results. Therapists can provide survivors with unique exercise programs they can perform independently at home.
However, these programs may often become tedious and cause individuals to lose motivation to exercise. To prevent this from happening, therapists may suggest using home therapy programs to keep survivors engaged.
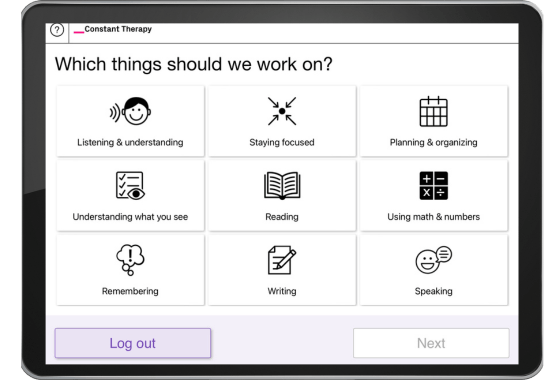
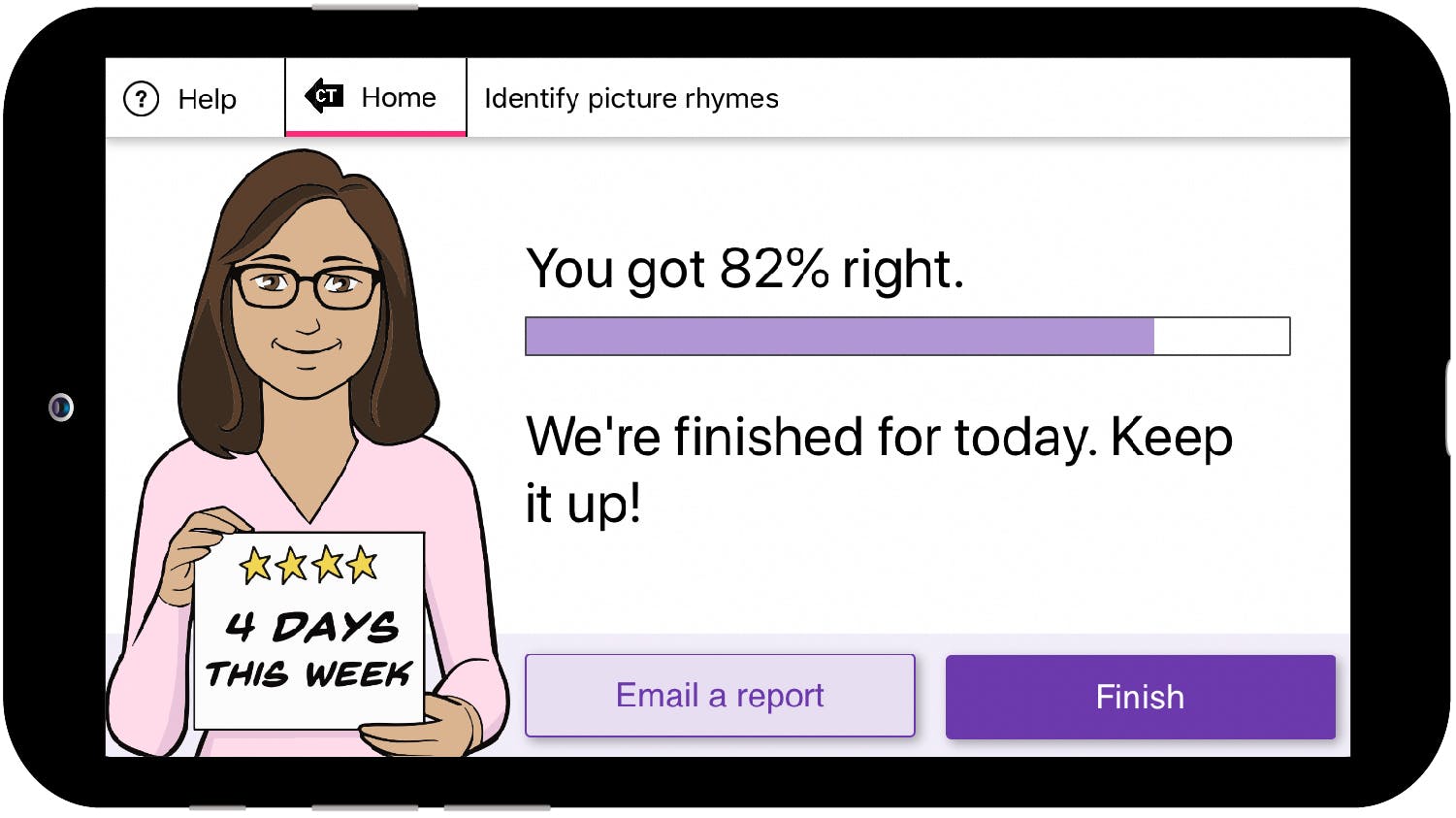
For example, the CT Speech and Cognitive Therapy App provides access to speech and cognitive exercises that are helpful for individuals with apraxia of speech. Therapists can use the app to assign appropriate exercises and/or the app can assess the individual and assign exercises based on current areas that need improvement.
Overcoming Apraxia After Brain Damage
Apraxia is a motor disorder that makes it difficult to perform purposeful movements such as speech or activities of daily living. This condition occurs following damage to areas of the brain in charge of motor control. By activating neuroplasticity through exercise, however, it may be possible to treat apraxia and regain muscle control and coordination.
We hope this article helped you understand the various types of apraxia after brain damage and how to boost your recovery.