Pediatric stroke is a rare condition that affects nearly one thousand children in the United States each year. Often, the road to recovery after a pediatric stroke is difficult. Fortunately, children’s brains are adaptable, allowing many pediatric stroke survivors to achieve a partial or even complete recovery.
This article will explain the causes and symptoms of pediatric stroke. Additionally, details regarding how to promote an optimal recovery are included. Use the links below to jump directly to any section.
- Perinatal stroke vs childhood stroke
- Pediatric stroke causes and symptoms
- Secondary effects of pediatric stroke
- Treatment for pediatric stroke survivors
Perinatal Stroke vs Childhood Stroke
A stroke occurs when the blood supply to the brain is compromised, either due to a blood clot in one of the brain’s arteries or as a result of a cerebral blood vessel rupture. The vast majority of strokes occur in individuals over the age of 65. However, in rare cases, children and even infants can also experience stroke.
Types of pediatric stroke can be separated into two categories based on age:
- Perinatal stroke: occurs from mid-pregnancy until one month after birth
- Childhood stroke: occurs between 1 month and 18 years old
Perinatal strokes are more common than childhood strokes, affecting up to 1 out of every 1,000 to 3,000 infants, while childhood strokes affect between 2.5 to 13 out of every 100,000 kids. Although about 25% of childhood strokes recur, there is less than a 1% chance that infants who experience perinatal stroke will have another.
Childhood stroke survivors generally have a better recovery outlook than infants who have had a perinatal stroke. While the prognosis for each infant or child is different, approximately 65% of perinatal stroke survivors have life-long neurological disabilities. On the other hand, individuals who experienced a childhood stroke often have a better prognosis than even adult stroke survivors, with only 20% of children experiencing long-term moderate to severe neurological impairments.
Pediatric Stroke Causes and Symptoms
There are a number of causes of pediatric strokes. Arterial ischemic strokes account for around 80% of all perinatal strokes, making them the most common type of pediatric stroke. On the other hand, approximately half of all childhood strokes are caused by brain hemorrhage (blood vessel rupture), while the other half result from ischemia (blood vessel blockage).
Pediatric strokes have a distinct set of causes. While the underlying cause of stroke in adults is typically high blood pressure or high cholesterol, the most common causes of stroke in children include:
- Sickle cell disease
- Congenital heart disease
- Blood clot disorders
- Weakened blood vessels
- Infections
Many of the signs of pediatric stroke are similar to the signs of stroke in adults. Symptoms typically include paralysis on one side of the face and/or arms, slurred speech, blurred vision, and/or severe headache.
However, these symptoms may be difficult to identify in infants. Perinatal stroke symptoms often include apnea (pauses in breathing), difficulty feeding, lethargy, and seizures, which are most common during the first three days after birth.
Unfortunately, about forty percent of perinatal stroke survivors do not display any initial symptoms. This means that the stroke is only identified as the child grows and developmental delays become visible.
Secondary Effects of Pediatric Strokes
Effects of pediatric stroke among young children usually present as delays in meeting developmental milestones, while older children may experience the loss of functions they had already developed. Overall, pediatric stroke survivors often experience many of the same secondary effects as adult stroke survivors.
Potential effects of pediatric stroke include:
- Delays in achieving developmental milestones such as rolling, sitting, and crawling
- Favoring one hand, especially before age 1
- Hemiparesis (weakness on one side of the body)
- Speech and language impairments
- Vision changes
- Behavioral and emotional changes
- Cognitive difficulties
Through rehabilitation, pediatric stroke survivors may be able to overcome these effects. However, severe strokes may result in other stroke-related disabilities, such as cerebral palsy, epilepsy, or learning disabilities. If a child displays any of the above symptoms, their doctor might refer them to a pediatric neurologist for further testing.
Treatment for Pediatric Stroke Survivors
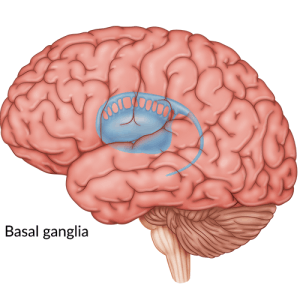
Activating neuroplasticity is the key to recovering from the effects of stroke, for both children and adults. Neuroplasticity refers to the brain’s natural ability to reorganize the connections between neurons (brain cells). This ability allows healthy, undamaged brain areas to assume control over functions previously associated with damaged areas. As a result, individuals can regain skills that had been lost or impaired due to stroke.
To activate neuroplasticity, children must engage in targeted, repetitive exercise. This is because repetitively performing tasks can stimulate the brain to begin adapting and constructing new neural pathways. Continuing to practice targeted exercises and activities on a regular basis can reinforce these pathways, eventually making the tasks feel almost second-nature.
Therefore, to promote a fuller recovery from stroke, it is important for children to participate in rehabilitative therapies. Furthermore, encouraging children to continue working on their therapy at home can improve outcomes.
The following are a few of the best therapies for pediatric stroke survivors:
Physical Therapy
After a pediatric stroke, the brain may no longer be able to effectively send and receive messages from the muscles. This may cause physical changes, such as movement problems, weakness, or spasticity (high muscle tone). Physical therapy can help restore the communication between the brain and the muscles to promote recovery.
A physical therapist can use a number of exercises and modalities to improve motor skills after stroke. Those with little movement may initially benefit from mental practice and passive exercises, while those with less severe impairments may work on active exercises and strengthening.
Occupational Therapy
A stroke can also affect a child’s ability to participate in their normal daily activities. Occupational therapists focus on increasing a child’s independence with daily tasks, such as getting dressed, feeding themselves, and participating in school.
Occupational therapy sessions may focus on rehabilitative techniques, such as stretching and exercises, or introducing compensation strategies, such as using adaptive tools. Environmental modifications, such as placing clothing in an easily accessible drawer, may also be recommended by occupational therapists to improve independence.
Speech Therapy
A stroke can affect a child’s speech and language abilities. Speech therapists can address all aspects of language and communication, from the physical components to the more advanced cognitive elements. Since communication skills grow throughout childhood, it is recommended to continue with speech therapy consultations even years after a pediatric stroke. This will help them continue to develop the skills they need as they age.
Speech therapists can also address feeding and swallowing issues. They may suggest modified diets (such as eating only relatively soft foods), but they are also able to work on improving the muscular mechanics involved with eating.
Behavioral Therapy
A stroke, especially one that occurs in the frontal lobe, can lead to behavioral challenges, such as aggression and impulsivity. This can make it harder for children to control their emotions and behavior.
A behavioral therapist can help pediatric stroke survivors learn more constructive behaviors and coping mechanisms. For example, to keep children from becoming overwhelmed and acting out, a therapist could create a structured routine that the child could easily follow. Behavioral therapists can also work on improving self-awareness.
Home Therapy
The above therapies are critical for helping children recover from stroke. However, encouraging children to practice the skills they learned during therapy at home in between sessions is vital for an optimal recovery.
While conventional home programs consisting of rote exercises can be beneficial, children tend to respond well to therapies that incorporate music and gaming, such as FitMi home therapy. As one FitMi user enthusiastically wrote:
“We have been using FitMi since January and we can see the difference with my niece!!…By using this system we were able to keep her on track and even GAIN MOVEMENT in her still paralyzed arm! MOVEMENT!!!!! This girl can now lift her hand to her mouth!!!!!!! We will continue to use our FitMi DAILY!!!!!!”
FitMi brings an element of gaming to rehabilitation and encourages individuals to challenge themselves and beat their high scores. As a result, many children complete their exercises without even realizing they are practicing therapy. Whether through a technology-based program or simply a written set of tasks, consistent, repetitive practice is vital to boost neuroplasticity.
Understanding Pediatric Stroke
Pediatric strokes are rare but serious conditions. Because a child’s brain is still developing, an early stroke has the potential to cause severe deficits later in their life.
Participating in consistent therapy, both at home and in the clinic, can boost neuroplasticity and promote functional improvements. While the road to recovery may be challenging, there is always hope for recovery through neuroplasticity.