Aggressive behavior after brain injury is often a direct result of damage to the areas of the brain responsible for emotion and behavior, such as the frontal lobe. Understanding behavioral changes that can occur after a head injury is essential to help your loved one manage day-to-day life.
Although managing aggressive behavior can be difficult for both the survivor and their loved ones, it helps to understand that it is usually not within the survivor’s control. Still, it is important for everyone involved to take the necessary safety precautions during aggressive situations.
This article will discuss how a brain injury can cause aggressive behavior and effective coping strategies for both TBI survivors and caregivers.
Use the links below to jump straight to any section.
Causes of Aggressive Behavior After Brain Injury
After a head injury, survivors can experience a variety of secondary effects. Depending on the areas of the brain affected, these effects can be physical, cognitive, and/or behavioral.
One area of the brain that is frequently associated with behavioral changes after TBI is the frontal lobe. The frontal lobe plays a crucial role in reasoning, problem-solving, and impulse control, all of which are necessary for regulating one’s behavior. When the frontal lobe sustains damage, it can impair behavioral skills, leading to aggressive and irrational behavior.
Studies show that 30% of frontal lobe injury survivors experience aggressive behavior. It most commonly appears during the first few weeks after the initial injury, a time period known as the acute phase. According to the Rancho Los Amigos Scale (a popular clinical scale used to measure cognitive recovery after brain injury), aggression can be characterized as a typical part of the recovery process.
In this early stage of recovery, survivors may also experience post-traumatic amnesia or disinhibition. Individuals with post-traumatic amnesia often struggle with memory and exhibit uncharacteristic behaviors. Similarly, individuals with disinhibition lack the ability to control inappropriate behaviors, often leading to risky behavior and poor decision-making after brain injury.
Many survivors are also at risk of entering a temporary state of delirium, where they have minimal to no control over their emotions and behavior. This delirium is often a symptom of frontal lobe damage.
While there are many correlates between frontal lobe injury and aggressive behavior, it’s important to note that damage to other areas of the brain responsible for emotions and behavior, such as the hippocampus, can also cause aggressive behavior after brain injury. In fact, studies have shown that between 11 and 34% of all brain injury survivors display aggressive behaviors at some point during their recovery.
Therefore, even though it may seem as though your loved one is intentionally being aggressive, it’s important to understand that they are often not in control of their actions, especially in the acute phase of an injury.
Aggressive behavior after brain injury can range in severity, from mild to extreme, and should be taken seriously. If you or your loved one are a victim of domestic violence or abuse, it is crucial to take action to protect yourself by calling the domestic abuse hotline in your area. For individuals residing in the United States, you can call 1-800-799-7233.
Understanding the Triggers of Aggressive Behavior After Brain Injury
Aggressive behavior can often be displayed physically or verbally. While it may seem like aggressive behavior is sporadic and sudden, it is usually triggered by emotional or physical discomfort. Survivors of TBI are often experiencing significant changes in their daily lives, and may no longer be able to participate in valued activities. This can be very frustrating, putting a strain on your loved ones’ emotions. When this frustration is combined with other less than ideal circumstances, your loved one may be more predisposed to aggression.
Understanding the triggers of aggressive behavior after brain injury can help you and your loved one find effective management and prevention techniques. Common triggers that can contribute to aggressive behavior after brain injury include:
- Overstimulation
- Depression
- Pain
- Fatigue
- Low glucose (sugar) levels
- Hunger
- Unrealistic goals and expectations
- Lack of independence or control
- Disability
- Perceived insults
Individuals may also struggle with the activities of daily living, such as eating and bathing, and may have difficulty asking for help. Identifying and if possible avoiding common triggers is the first step toward overcoming aggressive behavior after brain injury.
Coping Strategies for Survivors Demonstrating Aggressive Behavior After Brain Injury
As the brain heals, you may start to regain the ability to control your emotions and actions. While this can be challenging, it can be a stepping stone toward recovery. With the proper help and support, you can regain control of your emotions and reduce aggressive behavior.
Here are some coping strategies for TBI survivors that struggle with aggressive behavior:
- Take a break: When you feel that you are beginning to get agitated or angry, try to leave the situation. Find a safe space where you can relax and recharge. This can help you stay calm in an intense situation.
- Reach out to others: Do not be ashamed or afraid to ask for help when you need it. Trying to overcome your aggressive behavior all on your own can be overwhelming and depressing. Let your loved ones know how you feel and ask for their help and support.
- Try to understand your behavior: You can ask your loved ones for help in understanding your behavior and deciphering your actions. A loved one may also be aware of common triggers for your aggressiveness, and can help you make a plan to avoid triggering situations. Pay close attention to their comments and suggestions on how to navigate your emotions.
- Apologize: Even though your behavior was not intentional, it helps to apologize to others and be honest. You can share how you feel and why you believe you feel that way. Listen carefully to your trusted friends and take notes as to what you can do better next time.
- Seek professional help: Along with these coping strategies, it’s important to seek professional help such as behavioral therapy, psychological counseling, and/or psychotherapy. Each treatment provides a unique approach to aggressive behavior after brain injury.
- Rest: If tiredness and fatigue are triggers for angry or aggressive behavior, it can help to rest and take naps when necessary. However, pay extra attention to make sure that daytime naps don’t interfere with your ability to sleep through the night, because appropriate sleep is essential for TBI recovery.
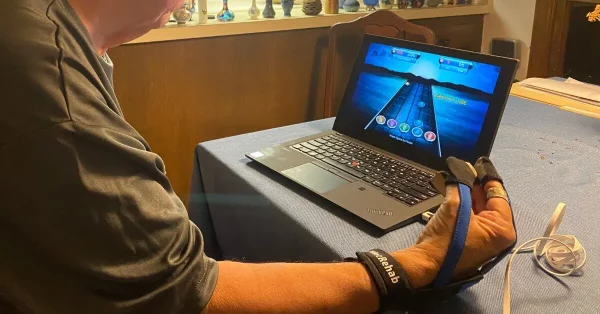
- Diet and exercise: If possible, try exercising for at least fifteen minutes a day and eat a healthy brain injury diet. A balanced diet can help reduce feelings of hunger, a common trigger of aggressive behavior. Exercise may also help elevate your mood and reduce fatigue after brain injury in the long term.
- Practice self-care and mindfulness: The practice of mindfulness involves intentionally being present in the moment. Take time each day to mindfully engage in a self-care activity. This could include taking a short walk, doing yoga, or praying or meditating. Taking even just a few moments each day to slow down and fully engage in an activity you enjoy can help you feel more regulated throughout your day.
Over time, as the brain heals, you may be able to regain control of your emotions and reduce outbursts. However, when an injury is severe, coping strategies and therapy may not be enough. In this case, medications such as SSRIs and other antidepressants may be helpful. These can help increase serotonin (the “happy hormone”) in the brain and reduce aggressive behavior.
Studies also show that a dopamine promoting antiviral medication known as amantadine can help individuals reduce aggression after brain injury. Although studies are limited, they show promising results and could be worth talking to your doctor about.
How Caregivers Can Help Defuse Aggressive Situations
Some survivors struggle with a lack of insight after a brain injury, especially in the early stages of recovery. Lack of insight refers to a cognitive deficit that makes it difficult to examine your own behavior.
As a result, survivors may not recognize irrational behavior or triggers. This can make it challenging for them to engage in effective coping mechanisms for their anger at first. Therefore, it’s important for loved ones to know how to help a survivor during this stage. Friends, family, and caregivers can provide guidance to help their loved one manage their triggers and aggressive behavior after brain injury.
To begin, you can try creating a peaceful and calm environment to help lessen exposure to your loved one’s triggers. This can also help you take better charge of a situation before it escalates. If a sudden outburst occurs, it helps to know what steps to follow to de-escalate the situation.
Here are some helpful tips to defuse an aggressive situation:
- Withdraw: Avoid arguing with the individual during an outburst. Rather, give them space by removing yourself from the situation. As you leave, inform them of the reason why you are leaving. This will allow the survivor to release their emotions and allow you time and space to process.
- Validate: Once the outburst has de-escalated and the individual has calmed down, it’s important to acknowledge their feelings. Kindly discuss their behavior with them while ensuring them that their feelings and emotions are valid and that you understand.
- Strategize: You can work with your loved one to avoid future outbursts by finding new strategies to release their feelings of anger. For example, instead of yelling, you can suggest they use a punching bag or a journal to write out their frustrations. You could also develop a code word to help the person realize they are acting out to help them manage their anger.
If an incident becomes violent, it’s important to always put your safety first. As the survivor relaxes, you can help them understand their behavior. Additionally, as you try to help your loved one cope with aggressive behavior, be sure to take the necessary safety precautions and take time for yourself.
Joining a caregiver support group and ensuring you have some personal self-care time can be vital. While being a caregiver can be rewarding, it may also be incredibly difficult. It is important to give yourself time and space to self-regulate before helping others regulate their emotions and behaviors.
Understanding the Link Between TBI and Aggression
While aggressive behavior after brain injury may seem intentional, it’s important to understand how it is caused and triggered. When the areas of the brain responsible for behavior like the frontal lobe are affected, it can impair behavioral regulation.
Fortunately, there are many effective coping mechanisms survivors can use to manage sudden outbursts and feelings of anger. It’s also important for friends and family to learn strategies to de-escalate aggressive situations while keeping their safety first.
We hope this article helped you and your loved ones understand how aggressive behavior after brain injury can occur, and how you can manage it.