Agitation is a common behavioral complication that can occur after traumatic brain injury. Typically, agitation develops during the early stages of brain injury recovery. However, this complication can also develop later in the TBI recovery timeline, affecting many daily functions and overall quality of life.
Agitation can be frustrating for both survivors and caregivers. Thankfully, there is hope for recovery as well as a variety of techniques to help manage agitation if it persists. This article will cover the causes and symptoms of agitation after traumatic brain injury as well as various techniques for reducing agitation and maximizing rehabilitation.
Table of Contents
Causes of Agitation After Traumatic Brain Injury
Agitation typically occurs in the early stages of brain injury recovery when the patient experiences post-traumatic amnesia. This condition is common after traumatic brain injury and affects around 30% of survivors. During this time, the individual often experiences memory loss as well as the inability to form new memories. The brain also has difficulty filtering information and attending to multiple forms of stimuli at once, which leads to overstimulation.
This phase can be extremely confusing and scary for the survivor since they are often disoriented to their surroundings and condition. Additionally, some individuals can become distressed when certain basic needs are not met in the moment. For instance, they may feel hungry, tired, or need to use the bathroom, but be unable to do so without assistance. These factors can contribute to severe agitation after traumatic brain injury.
Thankfully, post-traumatic amnesia and agitation are often short-lived, with most cases resolving within days or weeks. As we will discuss later in this article, however, agitation can last beyond this period of time and can also develop later in the recovery process.
Symptoms of Agitation After Brain Injury
Agitation is one of the many potential secondary effects that can occur following traumatic brain injury. Although this condition can present with a variety of symptoms, the most common symptoms of agitation include:
- Angry outbursts
- Impulsive or aggressive behavior
- Excessive talking or movement
- Restlessness
- Tension, anxiety, and irritability
- Sudden or intense mood swings
For example, individuals experiencing agitation may appear calm and content one moment but be suddenly triggered by an event in the environment, such as a loud sound or bright light. This can elicit unexpected, intense anxiety or frustration and cause the individual to lash out or have an outburst.
Additionally, agitation can present as a general discomfort or restlessness where the individual cannot get comfortable or find relaxation. When a survivor of traumatic brain injury is agitated, it is important for caregivers or family to remember that this is a secondary effect of TBI and not an intentional behavior.
As disorientation resolves and survivors progress through the later stages of recovery, these symptoms generally begin to diminish. When confusion decreases, survivors can regain control of their actions and, over time, these behaviors should subside. However, agitation sometimes continues even after post-traumatic amnesia disappears.
Why Agitation Occurs in Later Stages of Brain Injury Recovery
Although we’ve mainly discussed agitation in the acute state of brain injury recovery, agitation can also appear later in the recovery process, even after amnesia fades. Although persistent agitation is less common, it can have a negative impact on a survivor’s relationships and overall health if left untreated.
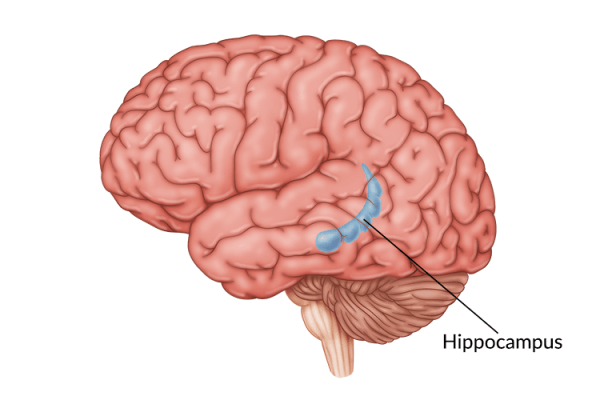
There are multiple reasons why agitation can persist or occur later in the recovery journey. One major contributing factor is the location and severity of the injury. For example, damage to the frontal lobe or amygdala can dramatically affect reactivity, decision-making, anxiety, and personality changes.
There are also many other conditions or situations that can contribute to agitation after traumatic brain injury. Some examples of these contributing factors can include:
Sensory Overload
Even after post-traumatic amnesia passes, the injured brain is still vulnerable to sensory overload. This vulnerability can cause a survivor to have a lower threshold for processing and reacting to stimulation from the environment, leading to increased agitation. Contributing factors for sensory overload include:
- Cognitive fatigue. The injured brain devotes most of its resources to repair itself. This means the brain has minimal energy left to process incoming sensory information such as sounds, light, noise, etc. As a result, even a small amount of stimulation can lead to sensory overload.
- Reduced concentration. Similarly, attention and concentration skills are limited after brain injury. Therefore, if too many things compete for a survivor’s attention, the brain will become easily overwhelmed.
- Increased stress. The stress, pain, and fatigue experienced following a traumatic brain injury can intensify sensory experiences and feelings, leading to increased agitation.
Sleep Disturbance
There is growing research to suggest that sleep disturbance is closely related to agitation after traumatic brain injury. Quality sleep is an invaluable part of the brain’s recovery process that is often negatively affected by traumatic brain injury. This can be due to both internal factors, such as the areas of the brain affected, and external factors, such as a loud hospital or rehab environment.
A widespread review of traumatic brain injury cases shows that 30-70% of individuals experience sleep disturbance following TBI. Sleep deprivation can cause an individual to be confused, irritable, and have difficulty processing information. Additionally, poor sleep can lead to impaired memory and decreased cognition.
These factors can increase agitation and slow the recovery process as the brain’s ability to heal is negatively impacted. Although more research is needed to fully understand the relationship between agitation and sleep deprivation, we know that effective sleep is a vital part of recovery following traumatic brain injury.
Depression and PTSD
Depression and PTSD are two conditions that are commonly experienced after a traumatic brain injury and can both be causes of increased agitation. Specifically, PTSD and depression can cause psychomotor agitation, which refers to unconscious, restless movements. Some examples of these movements include:
- Pacing a room
- Pulling at hair
- Wringing of the hands
- Tapping feet or fingers
- Talking rapidly
- Fidgeting
- Moving objects around unnecessarily
These behaviors are not concerning on their own, but someone with psychomotor agitation might do these things in a way that seems frantic or frustrated. These behaviors are characteristic of someone struggling with PTSD or anxiety and can often be triggered by events that remind the individual of the injury.
Additionally, increased agitation or irritability are common signs of depression and should be taken seriously. If you are experiencing signs and symptoms of depression or PTSD, talk with your provider about your concerns. They can help you find a treatment plan that is best for you and help connect you with useful resources.
Treatment for Agitation After Traumatic Brain Injury
Agitation can often be managed by a combination of treatments, and it is important to talk with your medical team to create a plan that is best for your specific symptoms and needs. This can include a combination of medication, cognitive-behavioral therapy, and environmental modifications.
In the early stages of recovery after traumatic brain injury, severe agitation may place the survivor at risk for bodily harm and sedative medications are sometimes prescribed to help alleviate this. These medications can be helpful in the short-term, but sedatives can suppress brain activity and slow TBI recovery. Therefore, they are often not a permanent solution for agitation.
If agitation does not decrease naturally, other medications such as antidepressants or anti-anxiety meds might prove useful. These can help manage symptoms of depression, anxiety, and general agitation to improve quality of life and increase participation in daily activities.
In addition, counseling and cognitive-behavioral therapy can help patients learn to process their emotions and cope with changes following traumatic brain injury. This includes reducing agitation and anxiety as well as learning techniques to help create new thinking patterns and mediate reactions to the environment. Cognitive-behavioral therapy is the most suitable for survivors who have improved their self-awareness or insight after brain injury.’
Tips for Managing Agitation After TBI
In addition to these treatments, there are other environmental or behavioral modifications you can make to help reduce agitation after traumatic brain injury. The following strategies may allow you to mediate agitation or prevent onset of agitation at all:
1. Limit Exposure
One way to avoid or reduce agitation is to limit exposure to stimuli such as intense lights, sounds, or other excessive sensory input. For example, turn off any devices that might make excess, unnecessary noise or bright light, such as the TV. It can also be helpful to avoid prolonged exposure to crowded, loud areas if possible. Additionally, it may be beneficial to invest in noise-canceling headphones so you can reduce stimulation in loud environments or situations if necessary.
Family members should avoid asking their loved ones too many questions at once, especially during the beginning of their recovery as this can be confusing and overstimulating. Speak briefly and clearly; anything more complicated can increase frustration and, consequently, agitation.
Another helpful technique is to modify your home environment to create a space to decompress. If possible, dedicate a specific room in your house with decreased lights, sounds, and stimulation where you can relax without distraction.
2. Understand Your Limits
Learn to monitor your feelings and emotions so you can identify when you are overstimulated or beginning to feel frustrated. A cognitive therapist can teach you how to recognize when you are getting agitated and help mediate these feelings.
Talk with your family and friends about things that are difficult for you to process and come up with a safe word you can use when your agitation increases. This allows you and them to modify behaviors or environmental stimulation before your agitation progresses and you experience sensory overload.
For friends and family, it is helpful to allow sufficient time for the survivor to process your words during conversation. It is also important to avoid crowding or sudden touch/grabbing. Utilize positive reinforcement and try to be encouraging of positive social interactions and behaviors.
3. Exercise Regularly
Consistent exercise releases endorphins that can reduce stress and agitation. Additionally, regular exercise can lead to improved outcomes and enhanced neuroplasticity-the brain’s ability to heal itself. The American Physical Therapy Association recommends 20-40 minutes of exercise 3-4 days per week to maximize recovery after traumatic brain injury and help with emotional regulation.
Meditation and deep breathing are also excellent ways to relieve stress and decrease agitation. In fact, research shows that taking deep, controlled breaths activates the parasympathetic nervous system, which calms feelings of anxiety.
To practice deep breathing, simply close your eyes, and slowly inhale through your nose. Let the air completely fill your lungs, then hold for three seconds. Finally, exhale slowly through your mouth. Repeat several times until you feel more relaxed.
4. Avoid Triggers
Agitation is commonly triggered by physical feelings such as hunger, thirst, or fatigue. If that is the case, try to take steps to minimize these feelings. For example, set a timer on your watch or phone every two hours as a reminder to eat. It is also helpful to take breaks from daily activities to avoid frustration or sensory overload, which can trigger agitation.
As we discussed earlier in the article, PTSD can be triggered when a situation or stimulus reminds the survivor of their injury or trauma. This can be extremely upsetting and increase agitation and anxiety. Learning what situations or events trigger these feelings can help you mediate agitation. Additionally, it can be helpful to talk with your therapist and develop a strategy to avoid or neutralize these triggers.
5. Practice Good Sleep Hygiene
Sleep plays a major role in both agitation and general recovery following traumatic brain injury. It can be difficult to achieve quality sleep after TBI as your circadian rhythm, or sleep cycle, is often affected. Furthermore, poor sleep can increase risk of depression and reduces both cognition and memory.
It is important to practice healthy sleep habits or “sleep hygiene” to maximize quality sleep and boost recovery. Here are several techniques to improve sleep hygiene:
- Create a consistent sleep schedule. Going to bed and getting up at steady, regular times can help improve your sleep cycle.
- Make a pre-sleep routine. Having a consistent routine before bedtime can help prepare your brain and body for sleep. This might include taking a warm bath or shower, reading, or listening to relaxing music.
- Optimize your sleep environment. Make sure your sleeping area is as quiet and dark as possible to minimize sleep disturbance. Avoid performing work or stressful activities in your sleeping area during the day to maintain a calming atmosphere.
Dealing With Agitation After Traumatic Brain Injury: Key Points
Agitation after traumatic brain injury typically occurs at the beginning of recovery when the brain is in a vulnerable state. It can also be a secondary effect of depression, PTSD, and sensory overload. In most cases, agitation will resolve on its own as the person progresses in their traumatic brain injury recovery journey.
If agitation does not resolve automatically, medication, cognitive-behavioral therapy, and other tactics can help mediate agitation and maximize quality of life. It is important to work closely with your healthcare team to find the best treatment plan for you.