A spinal cord injury can result in loss of bowel control, which may cause discomfort, pain, or waste-related accidents. By implementing a safe, sustainable bowel program, individuals with spinal cord injuries can learn to better control their bowel movements and improve their overall quality of life.
To help you understand how to set up a successful bowel program after spinal cord injury, this article will discuss:
- How spinal cord injury affects bowel control
- Goals of a bowel program for individuals with a spinal cord injury
- Key factors involved in establishing a successful bowel program
How Spinal Cord Injury Affects Bowel Control
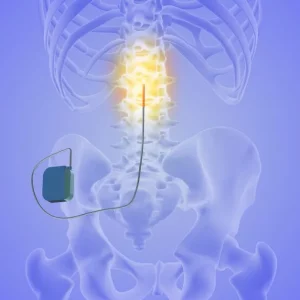
Neurogenic bowel dysfunction refers to the loss of bowel control after an injury to the nervous system, making it common following a spinal cord injury. In those with SCI, it occurs because signals from the brain can’t pass through the spinal cord damage and consequently, cannot reach the bowel muscles.
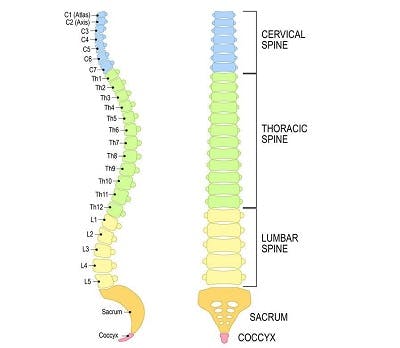
Neurogenic bowel dysfunction can be categorized into 2 general groups based on one’s level of injury. Level of injury refers to the bottommost region of the spinal cord where fully intact motor control and sensation exist.
Below, we’ll go over the main distinctions between the two classifications: ‘T12 and above’ and ‘L1 and below.’
T12 and Above
Spinal cord injuries at the T12 level and above result in reflexive bowels. This type of neurogenic bowel dysfunction describes when the anal sphincter remains involuntarily contracted. Because individuals with reflexive bowels experience difficulties relaxing the anal sphincter, they generally experience constipation and waste retention.
However, the reflex that allows bowel movements to pass when the rectum is full still works, so unplanned bowel movements may still occur.
L1 and Below
In contrast, spinal cord injuries at the L1 level and below result in flaccid bowels. This type of bowel dysfunction is characterized by loose bowel muscles due to the absence of the anal and bulbocavernosus reflexes.
Because the muscles are loose, individuals are more prone to accidents. Therefore, flaccid bowels are commonly associated with incontinence. Those with flaccid bowels should perform their bowel programs more frequently than those with reflexive bowels (daily, compared to every other day for reflexive bowels).
Now that you understand how level of injury can affect control over your bowel movements, let’s discuss the primary goals of a bowel program.
Goals of a Bowel Program for Individuals with a Spinal Cord Injury

Improving bowel function is reported to be one of the highest priorities among individuals with spinal cord injuries. Loss of bowel control following a spinal cord injury can have a significant impact on one’s quality of life. Complications associated with loss of bowel control after spinal cord injury include constipation, fecal incontinence, abdominal pain or discomfort, autonomic dysreflexia, and an increased risk of developing pressure ulcers.
Fortunately, there are several ways to effectively manage bowel problems to reduce their impact on one’s quality of life. A bowel program for individuals with spinal cord injuries generally focuses on:
- achieving regular bowel movements
- preventing constipation
- avoiding waste-related accidents
Individuals should work closely with their physician, rehab nurses, and occupational therapist to initiate a bowel program. Because every spinal cord injury is unique, a personalized treatment plan that targets each individual’s specific bowel complications is ideal.
In the following section, we’ll discuss some major factors involved in setting up a bowel program for individuals with spinal cord injuries.
Key Factors of a Successful Bowel Program for Spinal Cord Injury
Bowel programs will vary for each individual depending on the severity and location of their spinal cord injury, their lifestyle, and preferences. Generally, comprehensive bowel programs that involve several different interventions prove to be the most effective.
Below, we’ll go over 7 key factors that should be taken into consideration when developing a bowel program for an individual with a spinal cord injury.
1. Diet and Water Intake

What you eat and drink can significantly affect your bowel movements. For example, foods that are high in fiber help add bulk to your stool and promote movement throughout your digestive system. Likewise, drinking lots of water can help soften the stool, which makes it easier to pass and prevents constipation.
Generally, individuals with flaccid bowels want their stool to be a little drier to reduce the risk of accidents. However, this does NOT mean you should avoid drinking water, as dehydration can have severe consequences.
Individuals with bowel complications after a spinal cord injury should aim to consume about 15-20 grams of fiber and at least 1.5 liters of water a day.
2. Activity Levels
Your physical activity levels can also affect your bowel movements. Making an effort to move around throughout the day will help increase your metabolic rate and promote circulation. The faster your metabolism, the more efficiently your body can perform digestive functions.
3. Oral Medications

Sometimes, individuals with spinal cord injuries are prescribed medications to help manage secondary complications such as pain. However, these medications can come with adverse side effects that affect bowel movements such as constipation and diarrhea.
Additionally, some medications may help individuals manage bowel complications after a spinal cord injury. For example, individuals with constipation may use laxatives to help promote bowel movements. However, individuals can build a tolerance for them and may experience unfavorable side effects. As a result, they may not be ideal for long-term use.
Other oral medications for bowel management after spinal cord injury include bulking agents and stool softeners.
Ask your doctor which medications are most appropriate for you to be taking to help with bowel management.
4. Rectal Medications
Suppositories are medications that you insert into the rectum to deliver chemical stimulants that melt/dissolve with the body’s natural heat. They work by stimulating the nerves of the rectum so that individuals can regulate when they empty their bowels. Generally, only individuals with reflexive bowels should use a suppository.
Mini-enemas involve an injection of a liquid medication into the rectum, which can help soften the stool to prepare it to pass. These tend to be best used for those experiencing constipation.
5. Digital Stimulation

Digital stimulation relaxes and expands the anal muscles to enable individuals with spinal cord injuries to have regular bowel movements. It involves manually opening the anus with circular motions of the finger. This stimulates a bowel reflex that allows stool to exit the body.
One of your rehab providers will need to show you how to perform digital stimulation safely, as there are risks associated with it (tearing/bleeding and triggering autonomic dysreflexia, etc.)
6. Scheduling
Another significant factor to consider when implementing a bowel program for individuals following a spinal cord injury is scheduling. Ultimately, patients should aim to have a regular bowel movement around the same time every day or every other day.
By sticking to a schedule and performing the same tasks at around the same time every day, individuals can better predict when they should empty their bowels and prevent accidents.
7. Transferring
Because individuals with a spinal cord injury may have weakness or paralysis in their legs, core, and arms, it’s essential to find alternative ways to help them get on the toilet. This may involve using adaptive tools like a commode chair or raised toilet seat for convenience and safety.
It’s best to be seated during bowel movements so that gravity can help move the stool down the colon. However, individuals who cannot sit should lay on their left side as it corresponds with the direction of the colon.
Setting Up a Bowel Program for Spinal Cord Injury Patients: Key Points
Many individuals experience loss of bowel control following a spinal cord injury. As a result, they may experience constipation, incontinence, or abdominal discomfort. One of the most effective ways to reduce the impact of bowel problems on your everyday life is to set up a bowel program.
Bowel programs should be personalized to each individual’s functional abilities, lifestyle, and preferences. It often takes several weeks and a whole team of rehab professionals working together along with the patient to determine the appropriate bowel program for each individual, so don’t try to do this alone!
We hope this article provided some helpful insight on how to establish a bowel program for spinal cord injury patients. If you’d like to learn how to manage bladder problems after SCI, check out our article on regaining bladder control.