Brain injury and mental health have a complicated relationship. While TBI and mental health disorders can be unrelated, other times the two conditions may be linked.
This article will explain the connection between brain injury and various mental health concerns. It will also look at some of the most frequent psychiatric conditions that can arise after a TBI. A description of current treatments available for those suffering from brain injury and mental health disorders is also provided, as well as tips regarding how family members can offer support.
To jump ahead to certain sections, click on the relevant links:
- The Link Between Brain Injury and Mental Health
- Common Mental Health Disorders After Brain Injury
- Treating Brain Injury and Mental Health Together
- Supporting a Loved One with Mental Health Problems After Brain Injury
The Link Between Brain Injury and Mental Health
Brain injury significantly increases the risk of developing a mental health disorder. In a 2022 large-scale retrospective study, it was found that having a traumatic brain injury about doubled the likelihood of developing a psychiatric disorder.
Research has indicated that between 30-50% of those with a moderate to severe brain injury will develop a mental health condition. Mild traumatic brain injury can also increase a person’s susceptibility to mental health problems, with approximately 1 in 5 survivors experiencing mental health symptoms for up to six months after their injury.
Not all TBI survivors with mental health symptoms will be diagnosed with a psychiatric condition. For a doctor to diagnose an individual with a specific mental health condition, they must display all the traits of that disorder set out in the Diagnostic and Statistical Manual of Mental Health Disorders (DSM-5).
For instance, many TBI survivors suffer from extreme mood swings which also occur in bipolar disorder. But they may not receive a bipolar disorder diagnosis if they do not meet the other requirements.
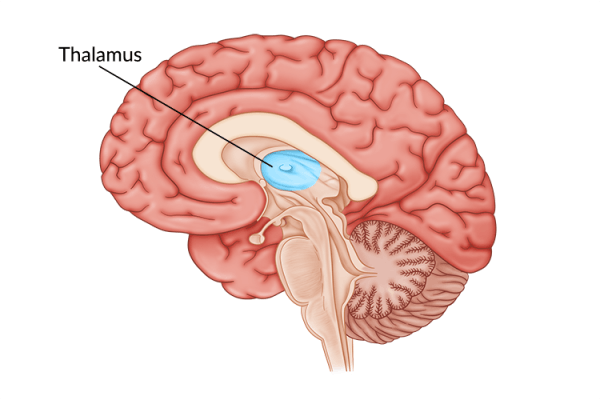
The link between brain injury and mental health is still being explored. However, neuroinflammation and post-TBI lifestyle changes may play a role.
Types of Mental Health Disorders After Brain Injury
While many individuals may experience mental health symptoms after brain injury, there are some survivors that present with all the necessary symptoms to be officially diagnosed with a mental health disorder. The following are some of the most common mental health conditions that individuals can experience after brain injury:
1. Major Depressive Disorder
Major depressive disorder (also known as clinical depression) is the most serious form of depression. It is among the most prevalent mental health disorders following brain injury, with brain injury increasing the risk of depression by 59%.
To receive a diagnosis of clinical depression, individuals must display 5 of the following symptoms over at least two weeks:
- Sad or irritated most of the day
- Loss of interest in activities that were once enjoyed
- Trouble staying asleep
- Sleeping more than usual
- Restlessness
- Difficulty concentrating and foggy thinking
- Feelings of worthlessness or guilt
- Suicidal thoughts
Unfortunately, many brain injury survivors exhibit at least a few of these symptoms. In fact, one study examining over 500 individuals with TBI reported that 53% met the criteria for major depressive disorder at one year post-injury, as opposed to only 6.7% of the general population.
Some causes of depression after TBI could include changes in brain chemistry due to the trauma, along with significant lifestyle changes due to the secondary effects of brain injury, such as being unable to return to work. Although depression is common after brain injury, it is often very treatable with a combination of talk therapy and medication.
2. Generalized Anxiety Disorder (GAD)
Generalized anxiety disorder, which is characterized by excessive worrying, is seen among 7.9 to 9.5% of TBI survivors during the first year after their injury. While there are a number of different types of anxiety disorders, a diagnosis of GAD is appropriate when 3 of the following symptoms are present more often than not during the previous 6 month period:
- Restlessness or feeling on edge
- Easily fatigued
- Trouble concentrating
- Irritability
- Muscle tension
- Sleep disturbances
Other anxiety disorders, such as panic disorder, are also seen among brain injury survivors. Treatment for anxiety disorders often involves a combination of medication and therapy, such as cognitive-behavioral therapy.
3. Post-Traumatic Stress Disorder (PTSD)
PTSD normally occurs after a significant, traumatic event like combat, assault, or near-death experiences. Individuals can also experience PTSD after a brain injury, especially since traumatic events can result in sustaining a brain injury. This is especially common among individuals in the military.
The symptoms of PTSD include:
- Involuntary reminiscing of the life-threatening event
- Avoiding people and places that remind an individual of their injury
- Emotional numbness and feeling detached from friends and family
- Overwhelming feelings of shame and guilt
- Constantly feeling on guard, irritable, or easily startled
- Anxiety and insomnia
- Angry outbursts
Many of these symptoms also overlap with other TBI symptoms. However, what defines PTSD is feeling immobilized by them.
According to a 2020 systematic review and meta-analysis, around 27 percent of brain injury survivors experience post-traumatic stress disorder. This makes TBI survivors around 2.68 times more likely to have PTSD than the general population. Potential treatments for PTSD include cognitive-behavioral therapy, mindfulness and meditation, and medications.
4. Mania
Mania, a condition characterized by periods of excessive excitement and hyperactivity, may also occur following TBI. To be diagnosed with mania, individuals must experience three of the following symptoms for over a week:
- Reduced need for sleep
- Rapid, excessive talking
- Racing thoughts
- Impulsive and risky behavior
- Abnormally high self-esteem
- Pacing or fidgeting
- Disorientation or disorganized thoughts
Although not in the diagnostic criteria, individuals may also experience hallucinations during a manic episode.
While mania is less common in TBI survivors than depression, it has been reported to affect between 4.2 and 9% percent of survivors. In addition, people with mania caused by TBI are less likely to experience euphoria and more likely to experience irritable moods and display aggressive behavior. Mania may be treated with medications such as Valproate and therapy.
5. Psychosis
Psychotic breaks are among the least common mental health disorders to appear after brain injury. While psychosis is not an official diagnosis in the DSM-5, many other mental health disorders, such as schizophrenia, include symptoms of psychosis in their diagnostic criteria. Individuals that do suffer from psychosis typically develop symptoms within the first year after injury. Sometimes symptoms have a delayed onset and may appear years later.
Symptoms of psychosis include:
- Auditory and visual hallucinations
- Paranoia or persecutory delusions
- Aggression
- Nonsense words
- Rapid speech
- Anti-social behavior
- Disorganized thoughts and behavior
Up to 9% of brain injury survivors experience a psychotic disorder at some point after their injury. Some of the most common symptoms of psychosis following a brain injury include auditory hallucinations and persecutory delusions.
It is important to recognize that psychosis, while serious, can be treatable with the right medications. Therefore, survivors and their loved ones should not feel ashamed and try to hide their symptoms. Rather, they should seek help from their doctor right away.
Treating Brain Injury and Mental Health Together
Treating a mental health disorder after brain injury will require support from a variety of professionals. If possible, it is best to seek the help of a neuropsychologist, a trained clinical psychologist who specializes in the effects of brain injury.
Since neuropsychologists are intimately familiar with both brain injury and mental health, they can recommend the most effective ways to heal the mind. Common methods that may be suggested include:
- Talk therapy
- Group therapy
- Mindfulness and meditation
- Cognitive-behavioral therapy
- Medication
Often, a combination of these treatments will be recommended. If there is not a neuropsychologist available in the area, other psychologists can also help. Just make sure they are familiar with the effects of brain injury on mental health.
Supporting a Loved One with Mental Health Problems After Brain Injury
Mental health disorders, especially depression, can be isolating conditions for those who experience them. Therefore, it is critical for loved ones to offer support during this time.
Some concrete ways to help a loved one experiencing mental health challenges include:
- Understand that their withdrawal isn’t personal. Many people with mental health issues might withdraw into social isolation. Depression in particular can make it difficult for people to connect on a deeper level, even with those they care about. If you notice your loved one pulling away, do not take it personally. Rather, tell the person that your love is unconditional, and that you are there if they need you.
- Do not try to “fix” them. Mental health issues can make life difficult. But as much as you might want to help your loved one, you can’t fix their problems for them. In fact, focusing all your efforts on curing them might actually backfire and cause the person to feel like their struggles are a burden to you. That is why it is crucial to be a compassionate listener, rather than always offering advice.
- Do not ignore the problem. On the other hand, it does not help to completely ignore the person’s symptoms and pretend they will resolve on their own. Without some form of treatment, most mental health problems will worsen. Therefore, it may be a good idea to gently start a conversation about treatment. For example, it may be helpful to mention something like, “I’ve noticed you have seemed pretty down lately, would you like to talk to someone about that?” The key is to emphasize that there is hope.
While these strategies will not eliminate difficulties, they can help make your efforts to support your loved one more successful. Being a family member or close friend of someone with a mental health disorder can be challenging. Seeking support from others in a similar situation through a support group may help you to better love and care for your loved one.
The National Association of Mental Illness has various virtual and in-person support groups throughout the US, and there may be other groups available in your specific area. Like the common saying, “you cannot pour from an empty cup”, it is important to ensure that you are emotionally and mentally well in order to best support your loved one experiencing a mental health disorder.
Understanding the Link Between Brain Injury and Mental Health
Brain injury and mental health disorders are frequently connected. That is why it is important for survivors to seek support for mental health after TBI.
Even if an individual is not displaying any symptoms at the moment, a good counselor can provide the tools necessary to stay mentally and emotionally healthy. With effective coping mechanisms, therapy, and medications as needed, individuals can learn how to live a contented and fulfilling life after brain injury.
For more, check out these Strategies to Overcome Depression and Mood Swings After Brain Injury.