Contractures are a common secondary complication of brain injury. They limit joint movement and can interfere with activities of daily living. Without appropriate management, tight muscles can become permanent contractures. Therefore, it’s essential to know why contractures occur and how to minimize their impact on your day-to-day life.
To help you understand contractures after brain injury, this article will discuss:
- What causes contractures after brain injury?
- What is the link between spasticity and contractures?
- How to prevent contractures after brain injury
What Causes Contractures After Brain Injury?
Movement is caused by the lengthening and shortening of opposing muscle groups. Contractures occur when muscle fibers consistently remain in a shortened state, causing a fixed tightening across the associated joint(s). This causes a decrease in range of motion and frequently limits one’s functional capacity.
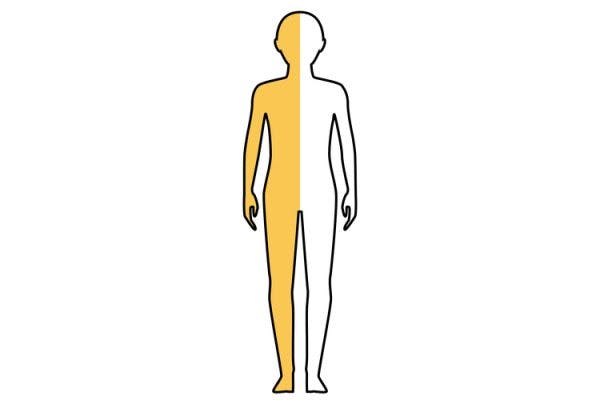
The most common areas where contractures develop after brain injury include the:
- Hips
- Shoulders
- Ankles
- Elbows
- Knees
- Wrists
- Hands
It is common for individuals with brain injuries to develop contractures across multiple joints, which places importance on early intervention and appropriate treatment.
Additionally, contractures can have both neurological and non-neurological causes. For example, a person whose arm is in a cast for months is at risk of contractures because, without movement, their muscles will tighten.
For individuals who have had a TBI, the most common cause of contractures is spasticity. We’ll discuss the relationship between these two conditions in the following section.
The Link Between Spasticity and Contractures

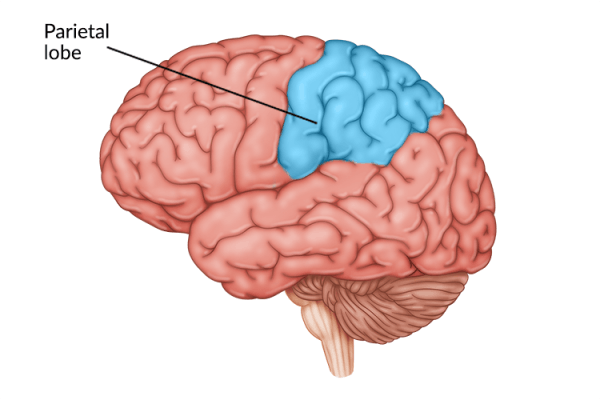
Spasticity is a condition in which the muscles are continuously contracted, causing tightness and muscle shortening. It is caused by damage to the part of the brain that controls voluntary movement. This damage leads to an imbalance of signals between the brain and the muscles.
Normally, motor signals from the brain travel down the spinal cord and through the peripheral nerves to reach the muscles and direct them to contract or relax. Following a brain injury, the transmission of motor signals may be disrupted, resulting in spasticity.
The longer the muscle stays contracted, the shorter the muscle becomes, until eventually a contracture (the fixed stiffening of the muscle fibers) sets in. This results in being unable to actively move the affected body parts. A true contracture is irreversible.
Therefore, to prevent contractures after brain injury, you will need to address the underlying spasticity.
How to Prevent Contractures After Brain Injury
While you may not be able to prevent all contractures after brain injury, you can prevent them from getting so severe that they become irreversible or require surgery.
One of the most effective ways to prevent the progression of contractures is through regular exercise and activity. Even if your contractures restrict you from using correct form, it’s important to make an effort to move each day. If you don’t, contractures will worsen and bone damage may occur.
Here are the best treatment methods for preventing contractures after brain injury:
1. Therapist Evaluation
The first step to preventing contractures after brain injury is to have a physical or occupational therapist evaluate you (depending on what body part is being assessed). They will determine whether any of your muscles are affected by spasticity and then develop a personalized rehabilitation plan. They may also recommend using heat and massage to help relax spastic muscles and relieve any associated pain.
If there is severe spasticity, they might recommend you try Botox injections first.
2. Botox Injections
Botox is a nerve-blocking agent that prevents the release of acetylcholine, a neurotransmitter that causes your muscles to contract.
It can help your muscles relax and stop painful spasms, which makes it a popular treatment option for spasticity. However, the effects will wear off in a few months. During that period, you can work on lengthening your muscles to minimize your spasticity, making progress that can carry over even once the Botox has worn off.
3. Orthotic Devices
Another intervention that can help you manage contractures after brain injury is wearing orthotic devices like splints and braces. They’re designed to provide structural support and hold your body in place to prevent muscles from further tightening.
An orthotic device can also help gently and passively stretch spastic muscles.
Depending on the affected body part and your tolerance to the orthotic, you may be recommended to wear it for short periods of time throughout the day, or for a longer period of time, such as overnight.
4. Passive Lengthening

Passive lengthening involves a therapist slowly increasing your range of motion by stretching the affected limb. This must be done gradually to avoid injury.
There are two main techniques therapists use to accomplish this:
- Manual stretching. The therapist stretches the muscle to its maximum length and holds it for a few seconds. This can only be done for a short amount of time every day, otherwise, the muscles can become damaged.
- Prolonged holding. This involves holding the joint in a moderate stretch for a prolonged period. It usually requires the use of a splint.
Typically, the best approach is a combination of these options.
5. Activating Antagonist Muscles
Another way to treat spasticity to minimize your chances of contractures is to activate or strengthen the muscle opposite the one contracted (the antagonist muscle). For example, if your bicep has spasticity, your therapist might have you strengthen your triceps.
The idea is, if the antagonist muscle can become stronger, it can counter the tightening of the agonist muscle and pull the joint through the full range of motion. This technique works best for patients who still can activate their opposing muscles and have minimal spasticity.
6. Contract/Relax

Another helpful way to treat spasticity and prevent contractures is to inhibit the stretch reflex.
The stretch reflex is a muscle contraction that occurs in response to stretching within the muscle. When a muscle lengthens, the muscle spindles are stretched and alpha motor neuron activity increases. This causes the stretched muscle fibers to contract.
This reflex normally protects the muscles from injury and tears, but it also makes them more difficult to stretch. To get around this, therapists recommend taking advantage of reciprocal inhibition. This occurs when the one muscle group activates and the brain inhibits the stretch reflex of the opposing muscle.
Therefore, to use this technique to stretch your spastic muscle, you must activate the opposite muscle. For example, if your calf muscles are tight, activate your shin muscles. Then, after a few seconds, you will relax that muscle and start stretching the spastic muscle.
This approach is effective but can be dangerous if not done correctly, so only try it under the supervision of your therapist.
7. Electrical Stimulation
Electrical stimulation involves placing electrodes over the skin where spastic muscles are located. These electrodes emit electrical currents that mimic signals from the brain to stimulate the affected muscle and activate movement.
8. Surgery
Finally, in some cases, surgery may be needed to correct otherwise irreversible contracture deformities. Contractures not only shorten muscles but also can damage bones and ligaments.
Surgery can help lengthen muscles and repair some damage that has occurred. If the bones have become twisted by the contracture, the surgeon will most likely need to straighten them.
Some of these surgeries have long and painful recoveries, so it’s best to take early action to prevent the need for surgery.
Brain Injury Contractures: Key Points
Contractures after brain injury can occur for several reasons. The most common causes of contractures are physical inactivity and prolonged spasticity.
Preventing contractures will require regular stretching. This can help elongate the muscle fibers and prevent spasticity from developing into contractures or prevent contractures from getting worse.
Finally, stay as active as possible. The more you keep your muscles and joints moving, the more flexible they can become.