When the hypothalamus becomes damaged after a brain injury, some survivors may feel too cold or too hot or may even alternate between the two. The hypothalamus plays a critical role in temperature regulation but when it’s been impacted, it may not be able to control or prevent body temperature from increasing or decreasing.
This article will discuss how a brain injury can cause changes in body temperature, along with some of the symptoms and management techniques to help regulate temperature.
How a Brain Injury Can Affect Body Temperature
To understand changes in temperature after brain injury, it first helps to know how temperature is regulated in the body.
Energy must be converted into heat in order to maintain a regular body temperature. Heat production depends on energy metabolism which is controlled by the hypothalamus. The hypothalamus is an area of the brain that contributes to many functions including the regulation of metabolism, appetite, and body temperature.
Normal body temperature ranges from 97.5°F to 98.9°F (or 36.4°C to 37.2°C). Brain temperature in particular depends on three primary factors: local production of heat, temperature of the blood vessels, and cerebral blood flow.
When the hypothalamus becomes damaged after a TBI, it may no longer be able to regulate body temperature and/or cerebral blood flow as well as before. This is important because without good cerebral flow the brain does not receive optimal levels of oxygen or nutrients to function at it’s best, making it more difficult for survivors’ brains to heal.
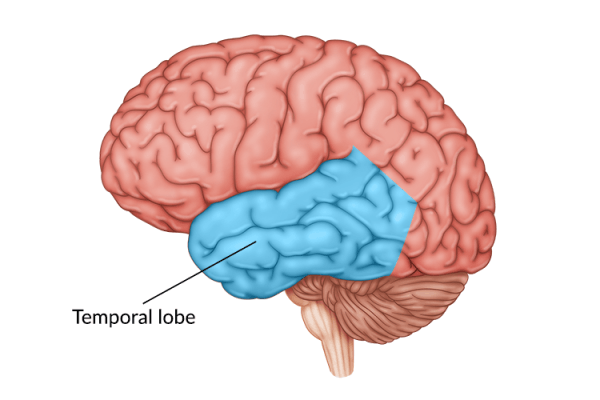
The somatosensory cortex is another region of the brain that contributes to the experience of temperature. Specifically, this part of the brain receives and processes sensory information including touch, temperature, and pain.
When the hypothalamus and/or somatosensory cortex are affected after a brain injury, changes in body temperature and brain temperature can fluctuate more broadly than before. However, temperature changes outside the normal range, can indicate more serious conditions. Seek emergency medical attention if you are concerned about changes in temperature regulation after brain injury.
Symptoms of Irregular Body Temperature After TBI
When the body feels really cold, the hypothalamus releases hormones that cause blood vessels to shrink or constrict. These vessels then direct heat in the blood to core organs and maintain body temperature. Therefore, when survivors are in a normal or even warm environment but still feel cold after head injury, it can indicate an issue with the body’s temperature regulation.
For example, an extreme drop in body temperature, below 95°F (35°C), can lead to hypothermia. In addition to feeling cold, survivors with hypothermia may experience:
- Shivering
- Delayed speech
- Slowed breathing
- Fatigue
- Confusion
When the body gets too hot, the hypothalamus releases hormones that cause the blood vessels to swell (dialate) allowing more heat to be carried out by the blood to the skin. This heat is then released into the air, allowing the body to cool and regulate temperature.
However, when this automatic function becomes impacted after brain injury it can lead to, in mild cases, heat sensitivity after TBI. In more severe cases, an extreme increase in body temperature can indicate a high-grade fever and/or hyperthermia. This occurs when the body temperature goes above 103°F (40°C).
Along with feeling hot, symptoms of hyperthermia may include:
- Fever
- Dizziness
- Nausea
- Excessive thirst
- Headaches
Survivors with hyperthermia may also experience fatigue and difficulty with cognitive functions, which can be further exacerbated in hot weather.
Therefore, while frequent hot or cold flashes can be common for survivors after a head injury, a prolonged period of extreme body temperature changes can indicate something serious. Consult with your doctor immediately if this is the case.
Managing Temperature Changes Post-TBI
Managing temperature regulation within your body can be challenging, especially when the weather is constantly changing. Fortunately there are techniques you can use to help regulate your body temperature in both hot and cold environments.
Tips to Stay Cool
When the weather outside starts to get warmer, especially during the summer, it helps to use techniques to cool down the body. This can include: draping a damp towel around the neck, wearing light-colored and loose clothing, and drinking lots of water. Staying hydrated is very important to prevent a heat stroke or any other heat-related illnesses, especially after a TBI.
Tips for Staying Warm
When the weather is getting colder or you’re feeling colder than usual, it can help to bundle up. Some tips include wearing extra layers of clothing such as sweaters and jackets, warm drinks such as tea or coffee, carrying a blanket with you, and taking a warm bath.
Sensory Retraining
Even if the body is doing all the necessary functions to regulate temperature, it’s possible the somatosensory cortex is not receiving or processing that information. This can cause survivors to struggle with perceiving irregular body temperature.
In some cases, sensory retraining (or sensory reeducation) may help survivors regain sensory function and be able to distinguish between temperatures. There are various simple, non-invasive sensory stimulation activities TBI survivors can try.
For example, you can soak a cloth in warm (but not hot) water and soak another cloth in cold water. Then, alternate holding each for about 30 seconds. This will help stimulate the brain to recognize and process temperature differences. Talk to your occupational therapist to learn more about sensory retraining.
Understanding Changes in Temperature Regulation After Brain Injury
The hypothalamus and the somatosensory cortex both contribute to temperature regulation. Damage to either structure can cause a variety of changes in the body’s temperature such as feeling extremely cold in warm environments, or vice versa.
While these are common effects after brain injury, persistent changes in body temperature can indicate more serious conditions such as hypothermia or hyperthermia. Seek emergency medical attention if you are ever concerned or have sustained high or low body temperatures.
Fortunately, there are techniques survivors can use to help with temperature regulation after brain injury, such as wearing cool or warm clothing. For survivors who struggle with sensory stimuli, sensory retraining may help. Lastly, keep track of any body temperature changes you experience. This information could be useful to a medical professional who can help you improve your body’s performance.