Crouch gait refers to an abnormal walking pattern commonly observed in individuals with cerebral palsy. While it can be worrisome when your child starts to walk irregularly, there are some interventions you can seek to encourage more typical walking patterns.
To help you understand what crouch gait is, this article will discuss:
- What causes crouch gait in individuals with cerebral palsy?
- Risks associated with poorly manage crouch gait
- Is crouch gait treatable?
- How to treat crouch gait in individuals with cerebral palsy
Causes of Crouch Gait in Individuals with Cerebral Palsy
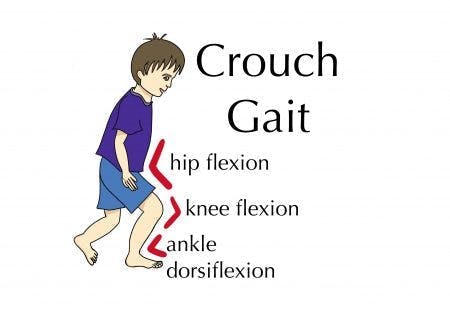
Crouch gait is an abnormal walking pattern that is characterized by:
- the upward bending of the ankles (ankle dorsiflexion)
- bent knees (knee flexion)
- bent hips (hip flexion)
This positioning gives the appearance of being in somewhat of a crouching position while walking, resulting in the name crouch gait.
Crouch gait is primarily caused by involuntary muscle contractions called spasticity. Spasticity is the result of disrupted communication between the brain and muscles. As a result, the muscles remain contracted for prolonged periods.
Cerebral palsy is caused by damage to the developing brain. Depending on the location of the brain damage, the child may experience spasticity in different areas of the body. While the brain damage that causes cerebral palsy does not get worse over time, the resulting spasticity can. Because the brain is unable to signal the affected muscles to relax, they remain contracted.
Consequently, when children with spasticity in their legs learn to walk, they may develop abnormal gait patterns like crouch gait.
In the following section, we’ll discuss the risks associated with poorly managed crouch gait.
Risks Associated with Poorly Managed Crouch Gait
Walking with crouch gait requires more energy than unaffected walking patterns, which often causes fatigue and joint pain.
Because of the additional strain on the muscles, joints, and bones, the body must work harder to maintain balance. Additionally, the continuous contraction of the ankles, knees, and hips results in constant pressure on some muscles while others remain underused. This muscle imbalance increases joint pressure and often results in chronic pain.
Without proper management for spasticity in the legs, individuals may be subject to additional complications including:
- uneven or distorted growth
- weakness of the hip and knee extensors and ankle plantar flexors
- subluxed or dislocated joints
- inability to walk
- compromised posture and stability
Now that you understand why crouch gait must be managed, let’s discuss whether it is possible to correct it.
Is Crouch Gait Treatable?
An abnormal walking pattern like crouch gait can be a major cause for concern. Fortunately, it is possible for individuals with cerebral palsy to improve their movements by engaging the brain’s ability to adapt: neuroplasticity.
Neuroplasticity allows functions affected by brain damage to be reorganized to healthy, unaffected regions of the brain.
The best way to activate it is through consistent and task-specific repetition. This helps reinforce demand for that function, which encourages the brain to make adaptive changes. The more you practice, the stronger the connections become.
Practicing walking with proper positioning frequently and consistently, rather than continually walking with crouch gait, can stimulate the brain to adapt and learn better walking habits until walking with a typical gait is second nature.
Learn more about neuroplasticity »
How to Treat Crouch Gait in Individuals with Cerebral Palsy

To correct crouch gait, individuals with cerebral palsy must treat its underlying cause: spasticity.
Generally, the earlier an abnormal gait pattern is identified, the easier it will be to correct.
Below, we’ll go over various interventions that may be involved in the treatment of crouch gait.
1. Orthotic Devices
It’s essential to fix poor form and positioning, even if that means your child may walk more slowly or effortfully while learning to correct crouch gait.
Orthotic devices like braces and splints provide structural support to promote proper musculoskeletal alignment, subtly stretch spastic muscles. and prevent further contractions.
Optimally, as the body and brain adjust to walking with a corrected gait pattern, individuals are able to gradually wean off of the use of their orthotic devices until they are no longer needed.
2. Botox
Botox is a medication that is injected into spastic muscles to temporarily relieve spasticity. It blocks the overactive nerve signals that cause muscle contractions.
The effects of Botox provide a window of opportunity for individuals to practice walking with proper form. Although its effects do wear off over time, the positive results achieved through consistently walking with correct form may carry over even after the medication has worn off.
3. Intrathecal Baclofen Pump
The surgery to implant a baclofen pump under the skin of the abdomen allows a consistent supply of baclofen to flow into the fluid surrounding the spinal cord.
Baclofen is a muscle relaxant that, like Botox, relieves high muscle tone. Because the drug is administered directly into the cerebrospinal fluid, you don’t need as high of a dose as you would if you were to take it orally. However, the pump does need regular refills, so baclofen pumps may not be the most ideal treatment option for children.
4. Selective Dorsal Rhizotomy
Selective dorsal rhizotomy is a surgical procedure that involves selectively cutting overactive sensory nerve fibers. Limiting the communication between the muscles and the brain can significantly reduce spasticity.
5. Single-Event Multi-Level Surgery (SEMLS)
SEMLS is the most invasive type of surgery for spasticity. It involves a surgical procedure that starts at the hips and ends at the feet, individually addressing each muscle imbalance and bone deformity along the way.
SEMLs can involve lengthening tendons, moving muscles, and altering bones. Fixing the alignment of the musculoskeletal system is able to significantly reduce spasticity without directly intervening with the central nervous system.
6. Physical Therapy
Lastly and most importantly, intensive physical therapy is essential for treating abnormal gait patterns like crouch gait.
Whether your child uses a brace, Botox, or gets surgery to treat spasticity, they must participate in intensive physical training to correct their gait.
The exercises performed in physical therapy sessions must be challenging and frequent to activate neuroplasticity in the brain and replace the existing walking pattern. Continuing with home exercises to carry over and solidify skills learned in therapy is also essential.
Crouch Gait in Children with Cerebral Palsy: Key Points
Abnormal walking patterns like crouch gait are common in children with cerebral palsy and without consistent management, they can worsen over time.
By detecting the abnormal walking pattern as soon as it arises and seeking early management, individuals can prevent the progression of spasticity and the development of detrimental habits. Long term, this will help minimize pain and pressure on the joints while improving balance and posture.
Hopefully, this article helped you better understand why crouch gait develops in individuals with cerebral palsy and how to go about treating it.