Traumatic brain injury is generally classified into two categories: focal and diffuse. A diffuse brain injury affects multiple areas of the brain, whereas a focal brain injury refers to a single area of localized damage.
Focal brain damage can lead to a variety of secondary effects, depending on the severity and location of injury. Fortunately, many of these effects can be improved with a combination of treatments, which often includes a rigorous rehabilitation program.
To help you better understand this condition, this article will discuss the causes, symptoms, and treatments for a focal brain injury.
Use the jump links below to help you navigate through this article:
What Is a Focal Brain Injury?
A traumatic brain injury is a broad term used to define a wide range of injuries or damage to the brain. Injuries can be focal, meaning they are confined to only one area of the brain, or they can be diffuse, which means the damage affects more than one area of the brain. In some cases, injuries can be both focal and diffuse, depending on the cause.
Some of the most common causes of focal brain injury include:
- Falls
- Sports injuries
- Motor vehicle collisions
- Blow to the head
- Brain lesion or blood clot that cuts off blood supply to a specific region of the brain
- Penetrating head wound
Focal brain injury can occur at the site of impact or on the opposite side of the impact, depending on how the injury is sustained. When focal brain injury occurs on both sides (site of impact and the opposite side) it is called a coup-contrecoup injury, meaning “blow and counterblow”.
Learn more about the difference between focal vs diffuse brain injury.
Classification of Focal Brain Injury
Focal brain injury can be classified into two main categories: open (penetrating) and closed. Open injuries refer to head trauma where the skull is fractured or penetrated. Closed injuries, however, do not involve skull fractures and are far more common.
Additionally, focal brain injury can be further classified into different categories based on the type of hemorrhage or bleeding caused.
Focal brain injury hemorrhages can include:
- Subarachnoid hemorrhage: The most common type of hemorrhage caused by bleeding into the subarachnoid space, located near the brain’s surface.
- Intraventricular hemorrhage: Bleeding inside the brain’s ventricles (fluid-filled structures located deep within the brain).
- Subdural hemorrhage or hematoma: A hematoma located between the covering of the brain (called the dura), and the brain itself.
- Epidural hemorrhage: Bleeding between the brain and the skull, creating increased pressure on the brain.
- Intracerebral hemorrhage: Characterized by bleeding in the cerebrum (the largest part of the brain responsible for functions such as coordinating movement, regulating temperature, and controlling emotions).
- Cerebral contusion: A type of intracerebral hemorrhage that refers to a bruise on the brain which can occur when the brain hits the skull.
Bleeding in the brain can increase the risk of complications and be life-threatening; therefore, timely treatment is crucial. Treatment will depend on the severity and the cause of the focal brain injury. For example, when a TBI is severe, surgery may be required to help relieve pressure from the brain and reduce bleeding or further damage.
Symptoms of Focal Brain Injury
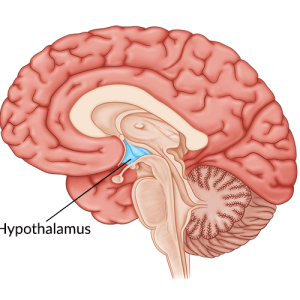
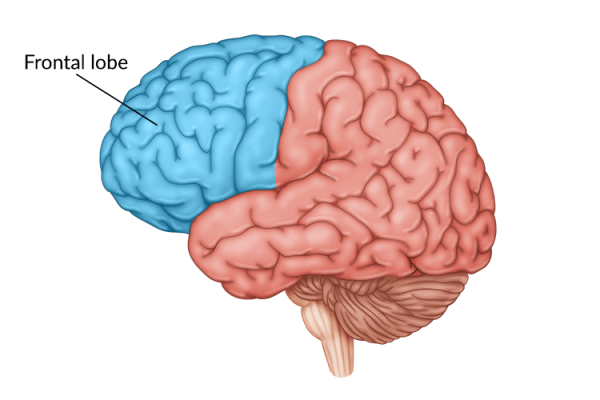
Symptoms of focal brain injury vary depending on the area of the brain affected. One region of the brain can control multiple functions. Therefore, even if only one area of the brain was directly impacted, a survivor may experience multiple different secondary effects or deficits.
For example, the frontal lobe is a large part of the brain that plays a role in behavior, language, and movement. When an individual sustains a frontal lobe injury, they may experience a combination of symptoms such as difficulty with speech and language or loss of voluntary movement.
Other symptoms of a focal brain injury can include:
- Sudden, intense headache
- Paralysis
- Numbness or tingling on either side of the body
- Vision changes
- Drowsiness or lethargy (difficulty staying awake)
- Seizures
- Mood or personality changes
- Nausea
- Onset of increased fear, paranoia, or depression
While all symptoms of focal brain injury require urgent medical care, some symptoms may signal a life-threatening hematoma, a collection of blood on the brain. One type, a subdural hematoma, can occur from both diffuse and focal brain injury and requires immediate medical intervention.
For example, during a car accident the initial blow to the head may only cause focal damage. However, other secondary injuries such as oxygen deprivation caused by a hematoma can lead to more widespread damage throughout the brain. Studies show that brain inflammation after TBI is not only restricted to focal lesions, but can also spread to remote areas of the brain and persist for weeks or even months following the injury.
Therefore, all symptoms of a TBI should be taken seriously and medical treatment should be sought out as soon as possible.
Can Surgery Help Treat Focal Brain Injury?
Initial treatment of focal brain injury will involve monitoring and stabilizing the individual to ensure no life-threatening complications develop. For example, if there is swelling in the brain, doctors may need to perform emergency surgery to relieve the pressure.
In severe cases, focal brain injury may require a decompressive craniotomy. This type of surgery involves removing a bone flap (a portion of the skull) in order to access the brain underneath. Once treated, the bone flap is reattached to the skull with metal plates and screws.
In other cases, a craniectomy may be required. Unlike a craniotomy, the bone flap is not immediately replaced after surgery in order to allow pressure on the brain to continue to resolve. Instead, individuals are required to wear a helmet to provide protection to the brain until the bone flap is replaced, usually around 6 weeks after the initial surgery.
While both types of surgery can be helpful, there is a rare complication after removing a piece of the skull known as “Syndrome of the Trephined.” This syndrome is associated with sensorimotor deficits and neurological deterioration.
Symptoms of Syndrome of the Trephined can often include:
- Headache
- Ringing in the ears
- Fatigue
- Loss of motivation and/or concentration
- Sensitivity to noise and vibration
- Anxiety or depression
There may also be other motor, cognitive, and language deficits associated with Syndrome of the Trephined. While this is a rare complication of decompressive surgery, all symptoms should be taken seriously. Doctors can provide survivors with more information regarding surgical interventions and other potential treatments for focal injury.
Treatments for Focal Brain Injury
After discharge from the hospital, treatment may include a combination of rehabilitation therapies to help manage any potential secondary effects from focal brain injury. This can include physical, cognitive, emotional, and/or behavioral effects, depending on the area(s) of the brain affected.
Rehabilitation is a key part of TBI recovery because it helps stimulate the brain and activate neuroplasticity – the brain’s ability to naturally heal and rewire itself. Neuroplasticity works by strengthening existing neural connections and creating new ones for a specific skill. It is best activated by massed practice of rehabilitation exercises, meaning high repetition is extremely important for recovery.
The more a skill is practiced, the more the brain will recognize that skill and strengthen its neural connections, which can help restore communication between the brain and the affected muscles.
Therefore, it’s important to practice high repetition of exercises and activities during all aspects of a rehabilitation plan, which can include:
Physical Therapy
Focuses on improving balance, strength, coordination, and overall mobility. Physical therapists understand how to assess a person’s unique needs and select specific rehab exercises that target those needs, such as gait training exercises for survivors that struggle with walking. They may also recommend a proper home rehabilitation program to practice in between therapy sessions.
Occupational Therapy
Helps survivors improve mobility while also finding safe and effective ways to perform activities of daily living such as eating and bathing. A therapist can provide individuals with adaptive equipment recommendations and/or rehabilitation exercises to help maximize independence after a focal brain injury.
Speech & Language Therapy
Assists individuals with a broad range of physical and cognitive communication disorders like impaired speech or difficulty swallowing. A speech-language pathologist can distinguish between different speech conditions and provide survivors with appropriate exercises. Speech therapy apps can be another great option for rehab between in-person sessions.
Cognitive Training
Cognitive training can works to improve any cognitive functions that may have been affected by a focal brain injury, especially damage to the frontal lobe. These cognitive exercises may help improve short-term memory, attention, problem-solving, and other executive functioning skills. Another great option for additional therapy both at home and on the go is cognitive training apps.
Home Therapy
Home therapy Keeps the brain stimulated in between therapy sessions to maximize neuroplasticity. To increase motivation and help survivors achieve massed practice at home, therapists may suggest using interactive rehabilitation equipment like FitMi home therapy. FitMi was designed to improve full-body mobility after a TBI. It provides survivors with interactive full-body exercises based on their level of ability.
Every focal brain injury is different, and every person’s recovery process will vary. Usually, the stronger the rehabilitation regimen, the higher the chances of improving function and lowering the risk of further complications. Therefore, establishing a proper rehabilitation plan is essential for TBI recovery.
Understanding Focal Brain Injury
Focal brain injury affects only one region of the brain, unlike a diffuse injury that affects multiple areas. However, depending on where the focal brain injury occurred, survivors may experience a wide range of secondary effects including physical, cognitive, and emotional effects.
Fortunately, these effects can be managed with a proper rehabilitation program to help stimulate the brain and activate neuroplasticity. There are also other treatments available to help minimize the risk of complications after a TBI. Consult your doctor to obtain a unique recovery plan that is safe and effective for your specific condition. We hope this article helped you understand the causes, symptoms, and potential treatments for focal brain injury.