Headaches after brain injury, also known as post-traumatic headaches, are one of the most frequently experienced effects of brain injury. While all traumatic brain injury (TBI) survivors are susceptible, individuals with mild brain injuries or concussions are more likely to experience persistent headaches after brain injury than those with more severe injuries.
This article will discuss the different types of headaches after TBI, as well as the best treatments that can help lessen their severity. Use the links below to jump directly to any section:
- Causes of Headaches After Brain Injury
- Types of Post-Traumatic Headaches
- Diagnosing Headaches After Brain Injury
- Treatments for Headaches After Brain Injury
- When Are Headaches After Brain Injury Dangerous?
Causes of Headaches After Brain Injury
In the year following a brain injury, between 14 and 58% of survivors experience post-traumatic headaches. While some individuals experience headaches immediately after brain injury, others can experience delayed-onset headaches.
Although the majority of headaches after brain injury subside within the first year, some individuals experience persistent post-traumatic headaches. A 2023 study looking at nearly 1,600 mild TBI survivors found that approximately 60% experienced headaches two weeks after injury. Of those, nearly half reported a persistent headache at 3 months post-injury, and just over a quarter continued to experience persistent headaches one year after their initial injury.
Post-traumatic headaches can occur for several reasons, including:
- Axonal injuries
- Changes in cerebral metabolism and blood flow
- Neuroinflammation
- Personal factors, such as genetic predisposition and an individual’s expectations
Vision changes, sleep disturbances, and stress related to TBI may also contribute to the development of headaches. Individuals who sustain a neck injury, such as whiplash, in addition to TBI may also experience headaches due to muscle tension or nerve damage.
Some individuals are more prone to experiencing headaches after brain injury, including females, those with a comorbid psychiatric disorder, or individuals with a history of headaches or migraines. Individuals with less severe brain injuries are also more likely to experience persistent headaches.
Types of Post-Traumatic Headaches
Post-traumatic headaches can be broken into several types. While tension-type headaches and migraines are most common, TBI survivors may also experience other types, such as cervical or cluster headaches.
Tension-type headaches are characterized by a dull, aching pain that may feel like the head is being squeezed. These headaches are often felt in the forehead, temples or back of the head, and are caused by tension in the jaw, facial, and neck muscles.
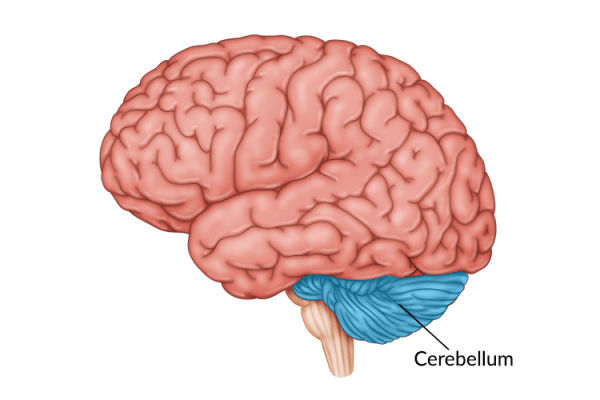
On the other hand, migraines occur when part of the brain is inflamed. This inflammation changes the way the blood flows to the brain, resulting in the dull, throbbing sensation most commonly associated with migraines.
Migraines are often accompanied by nausea, dizziness, and/or light sensitivity. Some individuals may also experience an aura, such as visual changes, before having a migraine.
Diagnosing Headaches After Brain Injury
The symptoms of post-traumatic headaches don’t always align with a specific type. In fact, many times individuals experience a combination of symptoms from several different types. Accurately identifying headache symptoms and type can help guide treatment, making it easier to manage the pain.
Therefore, it is crucial for individuals to be thorough when describing headache pain to their doctors. This can help doctors make the right diagnosis and offer the most effective treatment.
The acronym C.O.L.D.E.R can help individuals describe their headaches thoroughly:
- Character: Describe what the headache feels like. Is it a throbbing pain or more of a squeezing headache? Is it sharp or dull?
- Onset: How does the headache start? Does it start gradually or is it sudden and painful? Does it happen randomly, at a certain time of day, or after making a sudden movement?
- Location: Where does it hurt? All around the head or just in one area?
- Duration: How long do the headaches last?
- Exacerbation: Does anything make the headache worse? Maybe bending the neck forward, for example?
- Relief: Does anything make the headache lessen or feel better?
More details are better than less when determining an accurate headache diagnosis. Providing doctors with the answers to these questions, rather than simply reporting the occurrence of headaches, can greatly improve the chances of receiving the appropriate treatment.
Treatments for Headaches After Brain Injury
While each type of headache will require a different regimen, the most effective treatments tend to use a combination of medications and non-pharmacological interventions. Here are a few of the most commonly recommended treatments for headaches after brain injury:
Lifestyle Modifications
Adequate sleep and physical exercise can be key to helping relieve headaches after brain injury. Restorative sleep is essential for the brain to repair itself after injury. Therefore, lack of sleep can overwork the brain and delay the healing process, potentially making headaches worse. Studies have also shown that physical exercise, as well as participation in physical therapy as appropriate, can reduce headaches.
Dietary Changes
Maintaining a healthy diet and adequate hydration can help minimize headaches after brain injury. Try to avoid foods that trigger or exacerbate headaches, such as artificial sweeteners and alcohol.
A number of dietary supplements, including vitamin D, riboflavin, CoQ10 melatonin, magnesium, and omega 3 fatty acids, have also been recommended because of their potential to relieve headaches. However, survivors should always check with their doctor before adding supplements or making major dietary changes.
Non-Invasive Brain Stimulation
While lifestyle and dietary changes are often recommended initially due to their simplicity and ability to be easily integrated into one’s daily life, treatments such as non-invasive brain stimulation can also be effective. There are a number of non-invasive brain stimulation techniques, such as repetitive transcranial magnetic stimulation, that can be used to activate specific areas of the brain to reduce headaches.
Many studies have demonstrated the effectiveness of non-invasive brain stimulation, with some showing reduction in headache symptoms after only 1 week of treatment. If lifestyle and dietary changes don’t seem to be improving symptoms, survivors may consider consulting their doctor to discuss whether non-invasive brain stimulation would be appropriate
Cognitive-Behavioral Therapy
While still being studied, there is much evidence to support the use of cognitive-behavioral therapy for relieving headaches after brain injury. Cognitive-behavioral therapy involves changing patterns of thinking and behaving. For headache relief, cognitive-behavioral therapy strategies may include education regarding stress reduction techniques, practicing progressive muscle relaxation, and learning to implement coping strategies.
Medications
Pharmaceutical treatments are often used in combination with other treatment options to address headaches after brain injuries. Common medications include pain relievers such as acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen. Some evidence also suggests that antidepressants and antiepileptic medications can also help relieve post-traumatic headaches.
If possible, survivors should avoid strong medications such as opioids. This is because there is not strong evidence for their ability to relieve post-traumatic headaches, and TBI survivors have a heightened risk of developing opioid use disorders.
While medications may help, they should only be used as recommended. Taking too many medications can result in experiencing medication overuse headaches, exacerbating the frequency and/or intensity of headaches rather than providing relief.
Other Treatments
Depending on the type and cause of headaches, other treatment recommendations may include acupuncture, specialized prism lenses, peripheral nerve surgeries, or Botox injections. Individuals should consult with their medical team to determine which treatment(s) would be most effective for them.
When Are Post-Traumatic Headaches Dangerous?
Most headaches after brain injury are not cause for concern. As the brain heals, they usually decrease in severity and frequency.
However, there are cases when a headache can be a sign of a more serious condition. Individuals should call their doctor when a headache is accompanied by any of these symptoms:
- Fever
- Double vision (new onset)
- Vomiting
- Confusion
- Seizures
- Numbness or weakness
- Slurred speech
- Stiff neck (sudden onset)
Because these symptoms may indicate a more serious condition, such as a stroke, it is critical for survivors to call their doctor as soon as symptoms appear. This can ensure prompt treatment as necessary, if there really is a more serious underlying condition.
Understanding Headaches After Brain Injury
While headaches are one of the most common secondary effects of brain injury, many TBI survivors do not realize that there are effective treatments available that can reduce or eliminate their pain.
Instead, many suffer from post-traumatic headaches in silence, believing this is their new normal. Alternatively, they might have tried using different treatments or medications without positive results, not realizing that their headaches were stemming from their neck rather than their brain.
That is why it is essential to understand the different types of headaches after brain injury. Understanding the causes and types of post-traumatic headaches can empower survivors to get the right treatment as soon as possible.