Medications for spinal cord injury patients can provide relief for a variety of complications including pain, spasticity, depression, and bladder and bowel problems.
This article will go over some of the most commonly prescribed medications for spinal cord injury patients and their applications.
Risks of Medications for Spinal Cord Injury
It’s fairly common for spinal cord injury patients to take multiple medications to manage several complications. Studies report that 31% to 87% of SCI patients may be taking 5 or more medications.
While the use of multiple medications is a common standard of care in spinal cord injury management, it can cause adverse side effects that may negatively impact recovery.
For example, muscle relaxants can help relieve pain but also cause fatigue and dizziness. This can affect your motivation and ability to practice the exercises you need to improve. Therefore, finding the right balance of medications to help you manage complications and actively go about your everyday life is essential.
In the following sections, we’ll discuss how these commonly used medications work and their potential side effects. To jump straight to a specific section, click the links below:
- Corticosteroids
- NSAIDs
- Antidepressants
- Anticonvulsants
- Narcotic analgesics
- Antispasmodics and muscle relaxants
- Antibiotics
Medications for Spinal Cord Injury Patients

Medications can help improve quality of life after spinal cord injury by minimizing inflammation and providing relief from secondary complications.
You’re about to learn about 7 commonly used SCI medications, what conditions they manage, and their associated risks.
1. Corticosteroids
Corticosteroids are a type of medication that can help minimize damage in the early phases of spinal cord injury.
After spinal cord injury, the body activates the release of biochemical processes intended to stabilize the spinal cord. However, these are powerful chemicals that can increase damage to the spinal cord by reducing blood flow, increasing inflammation, overexciting the neurons, and inhibiting axon regrowth.
Corticosteroids like Methylprednisolone are powerful medications that can help minimize the effects of those secondary processes and reduce overall damage. However, its use is controversial due to its high risks and lack of standardization.
Common side effects of Methylprednisolone include vomiting, dizziness, anxiety, and insomnia.
2. NSAIDs
Non-steroidal Anti-Inflammatory Drugs (NSAIDs) like ibuprofen and naproxen are easily accessible medications that can help relieve pain after spinal cord injury.
Pain after spinal cord injury can vary from mild to severe, and those with mild to moderate pain will likely be recommended NSAIDs.
They help relieve pain and swelling by slowing the production of prostaglandins, which play a huge role in reducing the perception of pain.
3. Antidepressants
Depression after spinal cord injury is common and can result in loss of interest, inability to concentrate, lack of energy, and changes in sleeping and eating habits.
Fortunately, depression can often be treated with the use of antidepressants and psychotherapy. Antidepressants like SSRIs and SNRIs can increase neurotransmitter levels in the brain responsible for regulating mood and perception of pain.
SSRIs (selective serotonin reuptake inhibitors) increase serotonin levels by blocking its reabsorption in the brain. Serotonin makes you feel happy and helps regulate sleep and appetite.
SNRIs (serotonin and norepinephrine reuptake inhibitors) work similarly to SSRIs, except they also block the reabsorption of norepinephrine, which plays an essential role in regulating energy and alertness.
Before deciding anti-depressants are not for you, make sure to allow your body to adjust. The effects of anti-depressants are not immediate and generally take a few weeks to fully kick in.
4. Anticonvulsants
Anticonvulsants like gabapentin can help spinal cord injury patients manage neuropathic pain. Neuropathic pain is caused by damage to the nerves, which can affect the hyperexcitability of pain signals.
Anticonvulsants reduce pain by suppressing the overactive transmission of pain signals below the level of injury.
Common side effects of anticonvulsants include fatigue, dizziness, and loss of coordination.
5. Narcotic Analgesics (Opioids)
Individuals experiencing severe chronic pain after SCI may be prescribed a class of medications called narcotic analgesics or opioids.
These powerful pain relievers work by binding to opioid receptors in the brain and activating neurotransmitters that not only relieve pain but also help regulate mood, digestion, movement, and reward perception.
While opioids can be effective pain relievers, individuals can develop tolerance and addiction to them. This makes them ideal only for short-term use.
Common side effects of opioids include drowsiness, dizziness, and constipation.
6. Antispasmodics and Muscle Relaxants
Antispasmodics (also commonly called anticholinergics) and muscle relaxants can help reduce the effects of bowel or bladder problems and spasticity after spinal cord injury.
A spinal cord injury can disrupt the transmission of messages between the brain and body. As a result, muscles below your level of injury may involuntarily contract.
Antispasmodics and muscle relaxants help block the transmission of signals that cause muscle contractions.
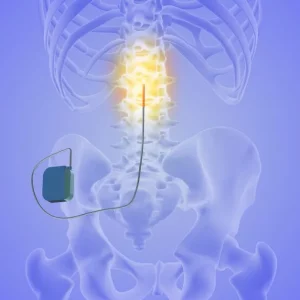
Muscle relaxants can be administered orally, through injection, or pumped into the spinal cord via surgical implant. Depending on how much of the body is affected by spasticity, some methods may be more ideal than others. For example, if contractions only occur in one leg, it’s better to directly inject the muscle.
It’s important to understand that these medications will only provide short-term spasticity relief because they do not address the underlying cause: nerve damage. For long-term relief, individuals should practice physical therapy exercises to stimulate neuroadaptive changes in the spinal cord.
Side effects of muscle relaxants include sedation, decreased blood pressure, and dizziness.
7. Antibiotics
Many higher level SCI patients have low lung capacity and weak coughs due to paralysis or weakness of major breathing muscles like the diaphragm, intercostals, and abdominals.
Individuals with poor coughing functions may struggle to clear secretions from the lungs. Therefore, they typically have a higher risk of respiratory infections like pneumonia. As a result, respiratory complications are the leading cause of death in spinal cord injury patients.
Antibiotics kill bacteria to prevent the spread of infection and can help clear the lungs of mucus buildup so that it’s easier to breathe and cough.
Medications for Spinal Cord Injury: Key Points

Medications can help minimize damage in the early stages of SCI and manage secondary complications like pain, spasticity, bowel and bladder problems, depression, and respiratory weakness.
While they can significantly improve your quality of life, medications should be taken with caution to avoid negative side effects that can interfere with your motivation and ability to pursue rehabilitation after spinal cord injury.
Hopefully, this article helped you better understand what types of medications may be prescribed after SCI and how they work. Good luck!
Photos from top to bottom: iStock/vadimguzhva/kiattisakch/nensuria