After a spinal cord injury, individuals may experience a condition called neurogenic shock. During neurogenic shock, the blood vessels expand, which causes unstable blood pressure, heart rate, and body temperature. This can significantly affect the flow of oxygen-rich blood throughout the body and requires immediate medical attention. With timely treatment, normal blood flow can be restored and promote optimal body functioning.
To help you better understand what neurogenic shock is, this article will discuss:
Causes of Neurogenic Shock
Neurogenic shock most commonly occurs following spinal cord injuries that disrupt innervation (the supply of energy) to the sympathetic nervous system. The sympathetic nervous system is responsible for activating the body’s “fight or flight” response. When activated, the body is on high alert: the blood vessels tighten (constrict), and blood pressure and heart rate increase.
The sympathetic nervous system is opposed by the parasympathetic nervous system, which is responsible for your “rest and digest” functions. When activated, the blood vessels expand (dilate), blood pressure and heart rate decrease, and digestion is stimulated.
Both systems are essential for appropriate functioning. Generally, the parasympathetic and sympathetic nervous systems alternate dominance throughout the day, depending on the situation, to support the body’s needs.
During neurogenic shock following a spinal cord injury, the loss of sympathetic innervation results in unopposed parasympathetic stimulation. In other words, the body’s relaxation response takes over without restraint.
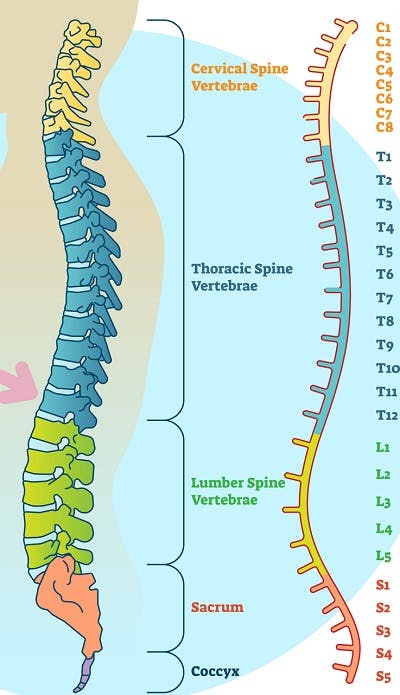
Because sympathetic innervation of the heart is associated with the T1-T5 levels of the spinal cord, neurogenic shock is most common in individuals with T6 or higher level spinal cord injuries. Individuals with cervical spinal cord injuries are more likely to experience neurogenic shock than those with thoracic SCIs. Additionally, the higher and more complete the SCI, the more severe the shock.
Although much rarer, it is also possible for individuals with spinal cord injuries below the T6 level to experience neurogenic shock. This is because sympathetic innervation of the blood vessels continues down to the L2 level of the spinal cord.
While neurogenic shock is most commonly associated with spinal cord injuries, it can also be caused by:
- Spinal anesthesia
- Guillain Barre syndrome
- Autonomic nervous system toxins
- Transverse myelitis
- Trisomy 21
- Skeletal dysplasia
- Tonsillopharyngitis
- Other neuropathies
In the following section, we’ll discuss common signs and symptoms of neurogenic shock.
Signs and Symptoms of Neurogenic Shock

Neurogenic shock generally lasts between 1-6 weeks after a spinal cord injury occurs. While it mostly affects the cardiovascular system, neurogenic shock can lead to permanent tissue damage if left untreated. Therefore, it’s essential to be aware of its symptoms and seek immediate medical attention.
Loss of sympathetic innervation causes the blood vessels to dilate, which leads to limited pressure pushing blood throughout the body. As a result, cells are not properly fueled with the oxygen and nutrients necessary for optimal body functioning.
Loss of sympathetic innervation may also cause blood to pool in the veins of the limbs. Instead of going back to the heart, blood may collect in the arms and legs. This creates a harmful cycle where less and less blood circulates throughout the body.
Common symptoms [1],[2] of neurogenic shock include:
- Hypotension: Low blood pressure (lower than 90 mm Hg systolic or 60 mm Hg diastolic).
- Bradycardia: Slower than normal heart rate (below 60 beats a minute).
- Body Temperature Dysregulation: Initially, vasodilation and the pooling of blood in the extremities (arms and legs) may cause warm, dry skin. Over time, however, hypothermia may develop due to heat loss.
These 3 symptoms can present themselves in a variety of ways, including:
- Fatigue
- Dizziness/ lightheadedness
- Weakness
- Confusion
- Blurred vision
- Nausea
- Fainting
- Shortness of breath
- Poor concentration
To avoid permanent tissue damage caused by insufficient circulation, symptoms of neurogenic shock should be addressed immediately. In the following section, we’ll discuss treatments.
Neurogenic Shock Treatment & Management
When blood pressure and heart rate fall too low, the body does not have sufficient blood supply to function properly. As a result, poorly managed neurogenic shock can lead to significant cardiovascular and neurological damage. Therefore, treatment for neurogenic shock focuses on restoring heart rate and blood pressure to normal levels.
Treatment for neurogenic shock generally involves:
- IV Fluids. IV fluids are the primary treatment for low blood pressure. They replenish fluid levels in the veins to help stabilize blood pressure.
- Vasopressors. If IV fluids prove ineffective, vasopressors can help tighten blood vessels and increase blood pressure. Commonly used vasopressors include norepinephrine, phenylephrine, dopamine, and epinephrine.
- Atropine. If your heart rate is low, your doctor may prescribe atropine. It helps normalize heart rate by inhibiting parasympathetic activity.
It’s also recommended by the American Association of Neurological Surgeons and the Congress of Neurological Surgeons’ Guidelines that mean arterial blood pressure (MAP) is maintained at 85–90 mmHg for the first 7 days following acute SCI.
Up next, we’ll compare and contrast the differences between two types of shock that may occur following a spinal cord injury.
Neurogenic Shock vs. Spinal Shock
Neurogenic shock and spinal shock are two separate conditions that are often confused for one another because they can both occur after a spinal cord injury. Additionally, they can also share symptoms including hypotension and bradycardia.
Unlike neurogenic shock (which predominantly occurs at the T6 level of injury or higher), spinal shock can occur following injury to any region of the spinal cord.
Neurogenic shock refers to a disruption of the sympathetic nervous system that affects tone in the blood vessels. Without sympathetic tone, blood cannot efficiently circulate throughout the body, which results in a decreased heart rate, low blood pressure, and temperature dysregulation.
In contrast, spinal shock results in the temporary loss of all motor, sensory, and reflex functions below one’s level of injury. It’s caused by inflammation and swelling of the spinal cord, which restricts blood flow below the level of injury. Once the spinal cord is stabilized and swelling dies down, individuals may gradually recover some reflexes, sensation, and motor control. This will primarily depend on the severity of the spinal cord injury.
Neurogenic Shock: Key Points
Neurogenic shock following a spinal cord injury causes loss of sympathetic (“fight or flight”) stimulation. As a result, the body’s parasympathetic (“rest and digest”) functions are unopposed, leading to vasodilation, decreased heart rate, and low blood pressure. Fortunately, there are effective ways to treat neurogenic shock and minimize the risk of secondary complications.
We hope this article helped you understand what neurogenic shock is and why immediate medical attention is necessary to stabilize cardiovascular functions.