When a survivor sustains orbitofrontal cortex damage, it can lead to unwanted behavioral changes. The orbitofrontal cortex is an area of the brain responsible for the cognitive process of decision-making, but it is also involved in other cognitive functions.
Behavioral changes after a brain injury can make it challenging for both the survivor and their loved ones. Fortunately, there are different ways to help manage orbitofrontal cortex damage.
This article will discuss how orbitofrontal cortex damage can interfere with behavior, and potential treatment strategies.
What Is the Function of the Orbitofrontal Cortex?
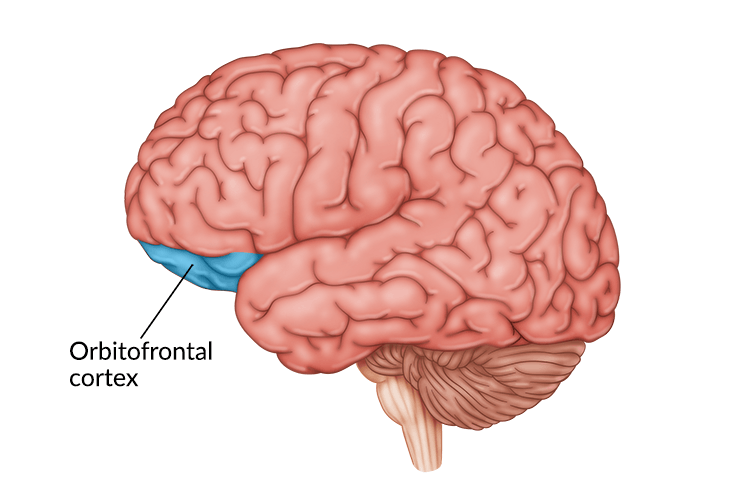
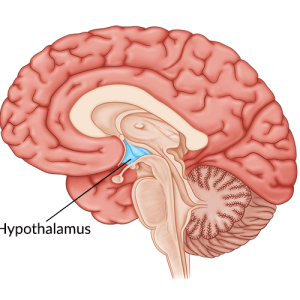
The orbitofrontal cortex is an area within the prefrontal cortex located in the frontal lobe. The orbitofrontal cortex sits just above the orbits (eye sockets) and is connected to the sensory and limbic system structures of the brain, which are involved in emotion and memory.
Neuroscientists believe that the orbitofrontal cortex contributes to several functions including impulse control, emotional reactions, social behavior, and value-based decision making. These functions can become impaired by damage to the frontal lobe and areas within it, such as the orbitofrontal cortex.
How Orbitofrontal Cortex Damage Can Cause Behavioral Changes
The orbitofrontal cortex plays an important role in helping us interact and socialize with others. Damage to this region can cause behavioral changes that interfere with the ability to interact with other people.
Five of the most common behavioral changes that can occur after orbitofrontal cortex damage include:
1. Poor Decision-Making
The orbitofrontal cortex plays an important role in value-based decision making. This means that it can help us narrow down simpler decisions and help us think through the value of each option. Recent studies have shown that the orbitofrontal cortex also helps individuals make predictions about their decisions based on prior experiences.
When this area of the brain becomes damaged, it can lead to poor decision-making, with or without predictions. Sometimes it may even seem like the survivor is insensitive about the consequences but motivated by immediate gratification.
2. Impulsive Behavior
Survivors may also experience a decrease in impulse control after an orbitofrontal cortex injury. Impulsivity, or disinhibition, can often lead to making rash decisions or displaying inappropriate behavior. For instance, some may feel comfortable sharing intimate or private information freely with both strangers and loved ones. Others may make rude remarks and become aggressive. Impulsivity can increase an individual’s risk of participating in reckless and/or dangerous activities.
3. Decreased Emotional Responses
Damage to the orbitofrontal cortex can also influence the way the body responds to certain stimuli or emotions. A decrease in emotional response can contribute to impulsivity and/or poor decision making. For instance, in a study that consisted of individuals with orbitofrontal cortex damage and individuals without damage, participants were presented with risky decisions. Many of those without orbitofrontal cortex damage showed signs of anxiety such as sweaty palms, but those with an injury did not. Individuals without damage also made less riskier decisions.
This helped researchers understand that the orbitofrontal cortex provides signals to the brain that help individuals make thoughtful decisions. Thus, when the orbitofrontal cortex becomes damaged, an individual struggles to receive warning signals about a decision, and often opts for the riskier choice.
4. Personality Changes
In the mid-1800’s, the case of Phineas Gage led scientists to discover that orbitofrontal cortex damage can also cause personality changes. Gage was a railroad worker who was using a tamping iron to pack explosives into a drill hole when the powder accidentally detonated. During the explosion, an iron bar shot through Gage’s left cheek, penetrated his orbitofrontal cortex, and exited through the top of his skull. Although he survived the injury, he quickly became known as “no-longer-Gage” due to the drastic change in his personality that was caused by trauma to the orbitofrontal cortex.
5. Other Behavioral Changes
Gage’s situation was a severe case of orbitofrontal cortex damage, less common than what most individuals experience. Still, many survivors and their family members have reported that their loved ones “seem different” in the way they behave or respond.
Orbitofrontal cortex damage is also associated with behavioral changes such as:
- Child-like behavior
- Aggressive behavior
- Apathy or low motivation
- Flat affect
- Lack of empathy or concern for others
When these behaviors put others at risk, an individual is often diagnosed with orbital personality. Although this condition is rare, it can often be misdiagnosed as acquired antisocial personality disorder. Fortunately, most survivors can improve their behavior with proper care.
It’s also important to note that not all behavioral changes are negative. In fact, some survivors may become more cheerful and engaging after a head injury. Orbitofrontal cortex damage can result in a variety of noticeable, and some unpredictable, changes. Consult with your doctor if you notice any new symptoms or changes.
Management Techniques for Orbitofrontal Cortex Damage
Treatment for orbitofrontal cortex damage may vary for every survivor. A psychotherapist is an expert in behavioral changes and can help you find the most suitable treatment. They may recommend a combination of different treatments.
Treatments for orbitofrontal cortex damage may include:
- Cognitive-behavioral therapy (CBT): focuses on training the brain to replace negative thoughts with positive ones. Therapists teach survivors new strategies and techniques to avoid potential harmful or uncomfortable situations, and help them to rationalize which behaviors are most appropriate. This can be especially helpful for individuals who experience impulsivity after orbitofrontal cortex damage.
- Social skills training: focuses on helping survivors improve social interactions. This can help survivors understand certain inappropriate behaviors and words in social settings. Social skills training can also increase empathy and emotional responses.
- Mindfulness meditation: focuses on being present in the moment. Shifting focus can help reduce stress and feelings of frustration. This not only helps relax the nervous system and reduce sensory overload, but it may also help grow the gray matter areas of the brain responsible for emotion regulation and mental flexibility.
All of these therapies encourage the survivor to practice emotion regulation and deliberate decision-making. When practiced on a regular basis, it encourages the brain to adapt through neuroplasticity. For example, when an individual with disinhibition practices taking time to weigh the options, it trains the brain to consider options more carefully when making decisions. While the effects do not happen overnight, there is hope that cognitive training like this can help individuals with orbitofrontal cortex damage to gradually improve decision-making.
Medication may not help treat orbitofrontal cortex damage directly, but it can help treat other possible symptoms from a frontal lobe injury such as pain or anxiety. ADHD drugs such as methylphenidate may also help reduce impulsive behavior. Consult with your doctor to see whether medication may be a safe and effective option for you.
How to Help a Loved One Cope with Orbitofrontal Cortex Damage
An orbitofrontal cortex injury can bring about many obstacles and life changes for the survivor. As a loved one, you can help them navigate these changes by being patient and understanding. Orbitofrontal cortex damage can result in some of the most challenging secondary effects of TBI for friends and family. The person you knew may speak or behave differently than what you were accustomed to, but it’s important to remember that their behavioral changes are often out of their control.
To help you cope with the changes and be able to provide support to your loved one after an orbitofrontal cortex injury, try to remember the following:
- Behavior changes are unpredictable: If your loved one says something inappropriate or reacts in an uncanny manner after a brain injury, remember that it is out of their control. Though it may seem they are aware of their own words and actions, it is unlikely that they are. The survivor may just exhibit more emotions and fewer inhibitions than pre-injury.
- Set kind boundaries: When your loved one says or does something rude or inappropriate, you can kindly speak to them and let them know. Avoid embarrassing them or making them feel bad. Simply help them understand why their actions or words were inappropriate for the situation.
- Do not give up: Overcoming behavioral changes from orbitofrontal cortex damage can be challenging for both you and your loved one, but do not be discouraged. Over time, with the proper care, it’s possible for the survivor to regain empathy and reduce inappropriate behaviors.
Lastly, remember to be patient. The brain is healing and your loved one needs time and rest to recover. Allow all the time and space necessary to improve their behavior and return to their daily activities. Consider joining a support group for loved ones of brain injury survivors to discuss challenges, receive emotional support, and learn from others’ experiences. Finally, a neuropsychologist can provide you with additional tips and information on how to help your loved one cope with orbitofrontal cortex damage.
Understanding Orbitofrontal Cortex Damage
Orbitofrontal cortex damage can affect emotions and behavior. Survivors may experience an increase in impulsive behavior or a lack of emotional response. While it may seem like these changes are irreversible, there is hope for recovery.
Cognitive-behavioral therapy and other treatments can help individuals manage behavioral changes after orbitofrontal cortex injury. It’s also important for loved ones to provide support and help the survivor learn how to improve their words and actions.
We hope this article helped you understand how orbitofrontal cortex damage can affect behavior, and the best ways to overcome it.