Paraplegia occurs when someone is paralyzed from the waist down. It most commonly occurs after a spinal cord injury, and it can create difficulty with daily activities such as walking or using the bathroom.
While paraplegia causes paralysis of the lower extremities, it does not affect upper body functions. As a result, spinal cord injury patients with paraplegia can learn adaptive techniques to maintain a great deal of their independence.
To help you understand the rehabilitation process for paraplegia, this article will discuss:
What Causes Paralysis from the Waist Down?
Generally, individuals who are paralyzed from the waist down have a mid-to-lower thoracic spinal cord injury. Sensation and motor control around the waist are typically innervated by the T7-T9 segments of the spinal cord.
Because signals from the brain cannot easily get past the level of the SCI, individuals often experience paralysis of functions innervated below their level of injury.
The severity of one’s spinal cord injury can significantly affect their degree of paralysis. Spinal cord injuries can be complete or incomplete. A complete SCI describes a lesion that transects the entire spinal cord, leaving no spared neural pathways. As a result, complete spinal cord injury patients will have no sensation or motor control below their level of injury, as there is no way for nerve messages to be transmitted past the injury level.
In contrast, an incomplete SCI describes partial damage that results in some neural pathways being spared. Less severe SCIs have more spared neural pathways, which is why some individuals can continue to move and feel areas innervated below their level of injury.
Now that you understand how spinal cord injury can cause paralysis from the waist down, let’s discuss potential complications.
What to Expect When You’re Paralyzed from the Waist Down
Individuals who are paralyzed from the waist down must understand how their lower body functions can be affected. This way, they can prepare for and prevent the progression of potential complications.
Below, we’ll discuss some of the most common outcomes of paraplegia:
1. Bladder and Bowel Dysfunction
Spinal cord injuries resulting in paralysis from the waist down can affect control of the muscles that make up the bowel and bladder.
These muscles are innervated by the lowest region of the spinal cord, the sacral region. As a result, it’s extremely common for SCI patients of any level of injury to experience bladder and bowel dysfunction.
Depending on one’s level of injury, the bladder and bowel muscles can become involuntarily tight or flaccid. Continuously constricted bladder and bowel muscles can result in urinary retention and constipation while continuously relaxed muscles can lead to leaking.
Management for bowel and bladder complications include:
- Adjusting your diet to include more fiber
- Using a catheter
- Implementing a bowel program to schedule bowel movements
- Taking medications to relax contracted muscles
- Getting surgery to enlarge the walls of the bladder
- Pelvic floor therapy to increase control of the bowel and bladder related muscles
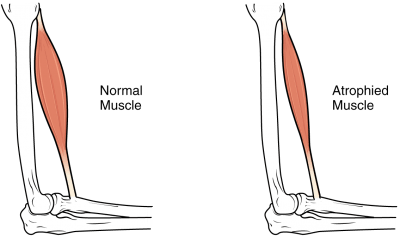
2. Muscle Atrophy in the Lower Extremities
Individuals who are paralyzed from the waist down may struggle with loss of muscle mass, also known as muscle atrophy.
Following an SCI, individuals may not be able to bear as much, if any, weight on their legs. As a result, the muscles tend to shrink from reduced use.
The principle ‘use it or lose it’ describes this perfectly. The more you use your muscles, the stronger they get. Similarly, lack of use can cause them to shrink. The human body is extremely adaptive and when it senses that a body part is not being used, it’ll make changes to conserve energy.
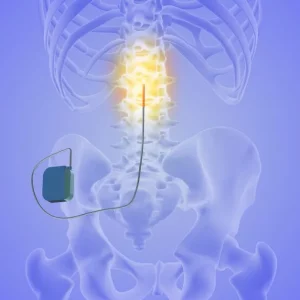
Some ways to help combat muscle atrophy include repetitively practicing leg exercises to stimulate neuroadaptive changes in the spinal cord. It is important to note that these exercises do not have to involve any extra weight, as the focus should be on the communication between your nerves and muscles, rather than the amount of resistance you’re able to use. Participation in functional electrical stimulation, which involves placing electrodes on the skin over targeted muscle groups to directly stimulate movement, can also help reduce muscle atrophy. This is something that your therapist could further instruct you in to optimally increase motor control and strength.
3. Sexual Dysfunction
Another potential outcome of paralysis below the waist is the loss of sexual functions. This can include loss of sensation, the ability to get an erection, and the ability to have an orgasm.
Individuals with sexual dysfunction should also be aware that they may be at risk for autonomic dysreflexia. Autonomic dysreflexia is characterized by a sudden rise in blood pressure due to stimulation below the level of injury. Because messages from the brain may be unable to travel below the injury site to regulate this response, individuals may experience feelings of panic, headache, and tightness in the chest.
Although autonomic dysreflexia is more common amongst individuals with a T6 level of injury or higher, it can also occur in individuals with T7-10 spinal cord injuries.
Every SCI is different, and speaking to your doctor can help you better understand what you can do to manage sexual dysfunction. About 80% of men regain some erectile function within 2 years of injury and most women are able to get pregnant.
4. Spasticity

Many individuals that are paralyzed below the waist experience spasticity in their legs. Spasticity occurs when the muscles involuntarily contract, which can cause stiff movements, spasms, and pain.
However, many SCI patients can also use spasticity in the legs to their advantage. For example, they can use the increased tone to help them stand up with their legs assisting in supporting them.
While spasticity may interfere with one’s ability to walk and control their movements, it’s generally a good sign of recovery because it indicates that spared neural pathways between the brain and body exist.
Minimizing the effects of spasticity typically involve physical therapy, muscle relaxants, Botox, or surgery. Muscle relaxants and Botox are used to temporarily minimize spasticity while physical therapy uses exercise and stretching to stimulate neuroadaptive changes in the spinal cord. Surgery for spasticity can involve manually lengthening the muscles and tendons, or making selective nerve incisions to reduce the excitability of spastic muscles.
Up next, we’ll discuss the mechanisms that make spinal cord injury recovery possible.
Can You Walk with Paraplegia?
Depending on the severity of spinal cord injury and the intensity of rehabilitation, individuals with paraplegia may be able to walk again. Personal motivation is also essential to regaining the ability to walk, as well as other functions, following a spinal cord injury.
The more spared neural pathways a patient has at their level of injury, the greater the potential for recovery. This is because spared neural pathways in the spinal cord may use neuroplasticity to rewire themselves.
Every time an individual practices a movement, the spinal cord is stimulated. Continuous repetition of a movement helps the spinal cord perceive a demand for that function, which promotes neuroadaptive changes. You may reteach your body how to walk again through repetitive, task-specific training.
Regaining the ability to walk can involve:
- leg range of motion and strengthening exercises
- the use of assistive devices (walkers, parallel bars, crutches)
- partial body weight supported treadmill training
- aquatic therapy
- spasticity management
It’s also possible for spinal cord injuries to initially appear worse than they actually are due to inflammation. Following a spinal cord injury, the body’s inflammatory response triggers an outbreak of biochemical processes that can cause swelling.
Excessive swelling can temporarily cut off blood flow in the spinal cord, resulting in the complete loss of reflexes, motor and sensory functions below the level of injury called spinal shock. Once swelling starts to die down and blood flow is restored, reflexes and functions may gradually start to return.
In the following section, we’ll go over how patients with spinal cord injuries can learn to optimize their independence as they pursue rehabilitation.
Maximizing Independence with Paraplegia

Because individuals with paraplegia have normal upper body functions, they can perform many activities of daily living independently.
At occupational therapy, patients with spinal cord injuries will have their functional abilities assessed. This may include range of motion, strength, and sensory testing, as well as a detailed evaluation of their ability to perform self-care tasks. Then, an occupational therapist will create a personalized rehabilitation plan aimed to improve mobility and maximize independence.
For example, patients with spinal cord injuries that are paralyzed from the waist down may learn how to get dressed in a wheelchair or how to get out of bed most efficiently and safely. An OT can also teach them how to use adaptive equipment like grab bars to make activities easier to perform.
By taking advantage of unaffected arm functions to help compensate for poor leg functions, individuals can continue to be self-sufficient as they work on rehabilitation.
Understanding Paralysis From the Waist Down: Key Points
Depending on the severity of your spinal cord injury, paralysis from the waist down isn’t always permanent. Because spared neural pathways in the spinal cord have neuroplasticity, it may be possible to relearn functions weakened by injury in many cases.
When individuals are paralyzed from the waist down, they’re susceptible to bowel and bladder complications, muscle atrophy, sexual dysfunction, and spasticity. By learning how to manage these challenges, individuals can optimize their quality of life.
Hopefully, this article helped provide you with hope for recovery after spinal cord injury. Good luck!