Abnormal posturing is a common outcome of severe brain injury. It refers to involuntary and abnormal positioning of the body due to preserved motor reflexes. The presence of posturing after TBI suggests a grim recovery outlook. However, prompt diagnosis and treatment may help improve outcomes.
To help you understand posturing after brain injury, this article will discuss:
- Types of posturing that can occur after brain injury
- Diagnosing posturing after brain injury
- Recovery outlook for posturing after brain injury
- Treatment of posturing after brain injury
Types Of Posturing That Can Occur After Brain Injury
There are 2 main types of posturing that may occur after a severe traumatic brain injury: decorticate and decerebrate posturing.
While each type of posturing has its characteristic features, they can present themselves differently in each individual. For example, some individuals may only show signs of abnormal posturing on one side of the body. Likewise, individuals may experience a combination of both types of posturing throughout the body. For individuals who do recover, abnormal posturing may still last for days or weeks following their severe brain injury.
Both types of posturing can be caused by damage to several regions of the brain; however, they often involve some extent of damage to the brainstem.
Below, we’ll discuss the defining characteristics of these two types of posturing.
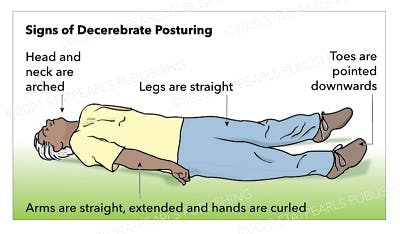
Decerebrate Posturing
Decerebrate Posturing. Contributed by Katherine Humphries
Decerebrate posturing is caused by damage to deeper brain structures, including the midbrain, pons, and diencephalon. Of the two types of abnormal posturing that may occur after a traumatic brain injury, decerebrate posturing is much more common.
Other names for decerebrate posturing include abnormal extension, decerebrate rigidity, extensor posturing, and decerebrate response.
This type of posturing is characterized by:
- Arched head and neck
- Straight and extended arms
- Bent wrists and curled fingers
- Straight legs
- Toes pointed downwards
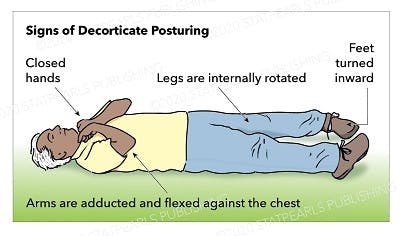
Decorticate Posturing
Decorticate Posturing. Contributed by Katherine Humphries
The second type of abnormal posturing that may occur after traumatic brain injury is called decorticate posturing. This is caused by damage to both hemispheres of the cerebral cortex, particularly if it involves damage to the internal capsules.
Although rarer than decerebrate posturing, decorticate posturing is generally associated with better survival rates. Additionally, this type of posturing is more likely to affect only one side of the body (left or right) than decerebrate posturing.
Decorticate posturing may also be referred to as abnormal flexion, decorticate rigidity, flexor posturing, or decorticate response.
This type of posturing is characterized by:
- Closed hands
- Internally rotated legs
- Adducted arms that are flexed at the elbows and wrists
- Inward turned feet
Now that you understand the major distinctions between these two types of posturing, let’s discuss how they are diagnosed.
Diagnosing Posturing After Brain Injury
To diagnose an individual with abnormal posturing after brain injury, physical examination is necessary. Individuals who present with abnormal posturing are typically unconscious, in a comatose state.
A physician will have the patient lie on their back with the arms relaxed at the side of the body. Then, a stimulus will be applied and the physician will observe for movement. Generally, abnormal posturing of the trunk and extremities occurs as a response to stimulation such as pain, but it may also occur without stimulation.
Usually, when an individual feels pain, they will cover their hand over the source or move their body away from it. What makes abnormal posturing unique is that an individual with decerebrate posturing will extend their arm no matter where the stimulus is applied.
When examining for decorticate posturing, bending of the elbows is generally slow and individuals should demonstrate normal withdrawal from the area where the stimulus is applied.
The following section will discuss the prognosis of individuals who demonstrate abnormal posturing after head injury.
Want 20 pages of brain injury recovery tips in PDF form? Click here to download our free ebook “15 Things Every TBI Survivor Must Know” (link opens a pop up for uninterrupted reading)
Recovery Outlook for Posturing After Brain Injury
Generally, the recovery outlook for individuals with abnormal posturing after brain injury is unpromising. However, there are instances where individuals regain consciousness and recover.
It’s suggested that 37% of individuals with decorticate posturing after head injury survive. In contrast, only about 10% of individuals who demonstrate decerebrate posturing survive. Additionally, it appears that individuals who are younger and admitted into the hospital within 6 hours of injury tend to be more likely to survive.
Up next, we’ll discuss the importance of timely treatment for abnormal posturing after brain injury.
Treatment of Posturing After Brain Injury
Immediate medical attention is essential for ensuring the best outcomes in individuals with abnormal posturing. Because every brain injury is unique, treatment will vary from person to person.
While an individual cannot be forced awake from a coma, early intervention can help minimize the progression of damage and secondary complications. Once the initial damage is stabilized, doctors may perform a series of tests to better understand the underlying cause of the individual’s brain injury and appropriately treat it.
Increased muscle tone related to abnormal posturing tends to be stronger while laying on one’s back, but it can decrease when sitting. As abnormal posturing may be more or less pronounced throughout the day, a physical or occupational therapist may attempt to position the individual in a sitting position when possible to limit muscle rigidity and optimize movement.
Posturing After Brain Injury: Key Points
Abnormal posturing after brain injury is indicative of severe damage to the brain. Individuals may demonstrate decerebrate or decorticate posturing, or a combination of both.
Generally, the recovery outlook for individuals with abnormal posture is poor. However, with timely medical attention, it is possible for individuals to awaken from their coma and recover from abnormal posturing.
We hope this article helped you understand the signs of abnormal posturing and what it means.