Pressure ulcers in spinal cord injury patients are extremely common as a result of impaired motor control and sensation. In fact, the reported annual incidence of pressure ulcers in individuals with SCIs is about 23-30%.
There are many different names for pressure ulcers. Therefore, if you hear the terms pressure sores, bedsores, or decubitus ulcers, know that they all refer to the same condition.
To help you better understand the link between pressure ulcers and spinal cord injuries, this article will explain:
- Why Pressure Ulcers are so Prevalent Amongst Individuals with SCIs
- What the 4 Stages of Pressure Ulcer Development are
- How to Prevent Pressure Ulcers After SCI
Causes of Pressure Ulcers in Spinal Cord Injury Patients
Impaired sensation is the leading reason why individuals with spinal cord injuries develop pressure ulcers. Prior to injury, people typically get the urge to move or shift positions after sitting or lying down for a long time.
Because spinal cord injury disrupts communication between the brain and body, the sensory signals that indicate there is too much prolonged pressure on a specific part of the body are not received by the brain.
As a result, individuals who lose sensation after spinal cord injury tend to no longer feel antsy or uncomfortable when sitting or lying in the same position for an extended period. Consequently, they remain in the same position, accumulating pressure.
When pressure accumulates for too long, blood flow to that area of the body is disrupted, which deprives the tissues of oxygen. This makes the skin susceptible to breakdown, known as pressure sores.
Additionally, individuals with higher-level spinal cord injuries are generally more likely to develop pressure sores because more areas of their bodies are susceptible to motor impairments and loss of sensation.
Other factors that can contribute to the development of pressure ulcers include:
- friction
- shearing
- moisture
- sepsis/ infection
- decreased autonomic control
- increased age
- malnutrition
- spasticity
In the following section, we’ll discuss the stages of pressure ulcer development.
Stages of Pressure Ulcers
Pressure sores are categorized into 4 stages, with stage 1 being the mildest and stage 4 the most severe.
Below, is a quick overview of each stage:
- Stage 1. A stage 1 pressure ulcer will present as redness or discoloration on the skin that doesn’t turn white/lighter when touched. This redness does not disappear within 20-30 minutes when pressure is removed and may be warm to the touch. However, the skin should still be intact (the skin is not broken).
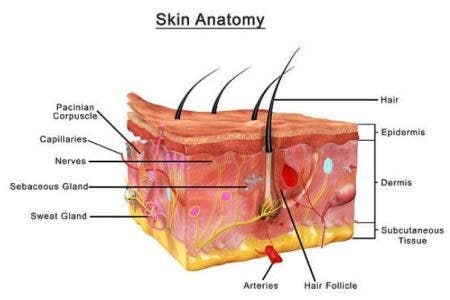
- Stage 2. Stage 2 pressure ulcers involve visible damage to the skin at the uppermost layer called the epidermis (the skin is broken). They’ll usually appear in the form of a blister or scrape, and there may be some drainage.
- Stage 3. Stage 3 pressure ulcers are deeper sores that extend into the subcutaneous layer. This is the bottommost layer of skin that is made up of fat and connective tissue.
- Stage 4. Stage 4 pressure ulcers are so deep that they involve damage to the bones and joints.
The earlier pressure ulcers are identified, the easier they are to treat. Likewise, the later pressure ulcers are identified, the greater the risk of additional complications including pain, infections, and in severe cases, death.
While a stage 1 pressure ulcer may only require a few days to heal, a stage 4 pressure ulcer can take anywhere from 3 months to 2 years. Damage to this extent sometimes requires surgical intervention to treat.
Up next, we’ll discuss the best practices for preventing pressure ulcers after spinal cord injury.
How to Prevent Pressure Ulcers in Spinal Cord Injury Patients
The development of pressure ulcers following spinal cord injury is preventable. Therefore, individuals must be made aware of their increased risk and learn how to be proactive about caring for their skin.
Proactive care to prevent the development of pressure ulcers is both cost- and time-effective compared to reactive care for treating an already developed pressure sore.
Below, we’ll go over some actions you can take to prevent getting pressure ulcers in the first place, and to stop the progression of an early stage pressure sore if you do get one.
1. Frequent Repositioning/Pressure Reliefs
This is the most important way to prevent pressure ulcers. It’s essential to move the body frequently throughout the day in order to ensure that excess pressure is not being put on any certain part of the body.
Reposition the body every two hours when lying in bed, and do “pressure reliefs” every 30 minutes when sitting up in your wheelchair. Each pressure relief should be held for about 1-3 minutes to be sufficient. Your therapists will be able to show you how to complete pressure reliefs properly.
Individuals with severe weakness or complete paralysis in their upper body will need a caregiver to assist them with repositioning and relieving pressure multiple times a day. For those who can operate a power wheelchair, the tilt and recline functions can be used for pressure relief when sitting up in the chair.
2. Daily Skin Inspections
It’s important to have regular skin inspections twice a day to spot pressure ulcers early and prevent them from progressing.
Keep an eye out for changes in skin color, temperature, texture, and moisture levels as they may indicate irritation beneath the surface.
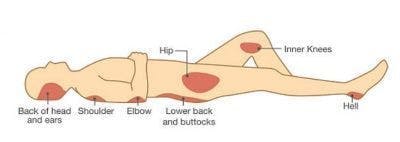
Pressure ulcers are most common in areas where the bones and skin are closely aligned such as the:
- elbows
- tailbone
- sit bones
- hips
- heels
- ankles
- knees
- back of head
- shoulders
Any of these bony prominences where you cannot feel is going to be susceptible to pressure ulcers.
One of the main goals of pressure ulcer management is to prevent the ulcer from growing and compromising the skin around it.
If you notice early signs of a pressure sore, try to remove all pressure on that area as much as possible and apply topical treatments as necessary. If it appears to be a stage 1 ulcer and does not improve within 2 weeks, then follow up with your doctor – do not wait for the wound to get worse! If it is already past the stage 1 phase, report it to your doctor immediately.
3. Cushioning
Making sure that areas susceptible to pressure ulcers are properly cushioned can help avoid friction.
Consider adding padding to your wheelchair seat as well as the footrests and armrests. Additionally, try to avoid sitting or lying on hard surfaces.
To prevent your ankles or knees from rubbing against each other when lying on your side, try placing a pillow in between the legs.
4. Skin Care
Making sure the skin is both clean and dry can help reduce the occurrence of pressure ulcers.
This helps ensure that irritants don’t accumulate on the skin. Excess moisture softens and causes swelling of the skin, making it more susceptible to breakdown.
Likewise, it’s important to keep the skin from getting too dry, as it may be more likely to tear.
There are several key recommendations to take care of the skin including:
- clean with warm (not hot) water
- only use mild cleaning agents to minimize the risk of irritating the skin
- avoid vigorously massaging over bony areas of the skin
5. Nutrition
There are many reasons why poor nutrition can increase the risk of pressure sores.
For one, individuals who are underweight have an increased risk of developing pressure sores due to thinning of the skin and reduced bone and muscle mass.
Our bodies need to consume essential vitamins and minerals to preserve the integrity of the skin. Low body weight and insufficient nutrients are linked to “slow and nonhealing wounds”.
Likewise, being overweight places additional pressure on the skin. Therefore, maintaining a normal weight through a nutrient-dense diet is ideal.
It’s also important to make sure that you’re drinking enough water. When you’re dehydrated, the skin becomes dry and loses elasticity, which increases the risk of pressure ulcers.
Spinal Cord Injuries and Pressure Ulcers: Key Points
Due to impaired motor control and sensation, individuals with spinal cord injuries have an increased risk of developing pressure ulcers.
Pressure ulcers can be costly to treat, force you to take time off work, and can be painful or even life-threatening. This complication of spinal cord injury may be common, but it’s also preventable.
By performing regular skin inspections, cushioning bony areas of the skin, maintaining a healthy weight, and making an effort to reposition the body throughout the day, individuals can minimize their risk of developing pressure sores and improve their quality of life.
We hope this article helped you better understand the risks associated with pressure ulcers following SCI and the most effective ways to prevent them.