Spasticity is an uncontrolled stiffening of muscles caused by a disruption of signals from the brain. The onset of spasticity after traumatic brain injury (TBI) is often rapid, occurring as early as one week following the brain injury.
Because spasticity is a problem originating from the brain, treatments must engage neuroplasticity, the brain’s natural repair mechanism, to be effective.
In this article, you will learn more about the causes of spasticity after TBI, plus the best ways to reduce it. You will also discover how to treat muscles that have been affected by spasticity.
Causes of Spasticity After TBI
Spasticity is associated with a condition called hyperreflexia, which is increased activity of the reflexes that normally occur in muscles. This reflex is actually a muscle contraction that occurs when the muscle is stretched or lengthened.
When you stretch a muscle, receptors within the muscle are activated which stimulate motor neurons to cause a contraction to prevent the muscles from stretching too far and tearing.
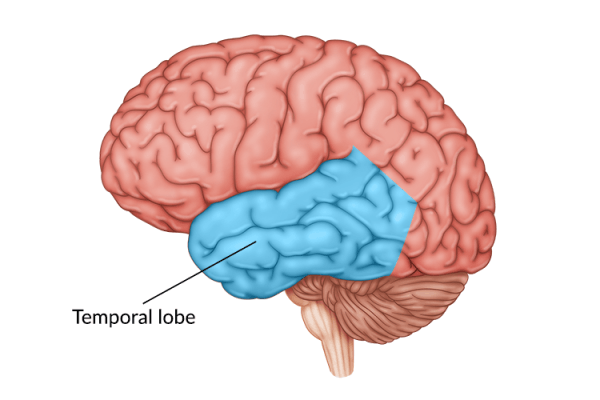
This reflexive process is overridden or controlled by the central nervous system (i.e. the brain and spinal cord). Normally, the muscles and the brain send messages to each other through the spinal cord.
However, after a brain injury, this communication is disrupted, which leads to an imbalance of signals. As a result, the reflex is never turned off, resulting in a constant state of contraction. This state is what doctors refer to as spasticity.
Signs and Symptoms of Spasticity

Spasticity after TBI primarily results in muscle stiffness. If the spasticity persists, the muscle adapts and is permanently shortened, leading to contractures and loss of mobility.
Other signs of spasticity can include:
- Muscle spasms
- Joint deformity
- Muscle fatigue
- Involuntary crossing of legs
Fortunately, you can prevent many of these with early intervention for spasticity.
Engaging Neuroplasticity to Treat Spasticity after TBI
The most effective way to overcome spasticity after TBI is to address the root cause. Since the cause of spasticity is poor communication between the brain and muscles, treating it must involve restoring that connection. You can do this by engaging a process known as neuroplasticity.
Neuroplasticity refers to the brain’s ability to rewire itself and create new neural pathways. This allows undamaged areas of the brain to take over functions from damaged ones.
These new pathways are formed when your brain gets stimulated by effortful, repetitive, therapeutic exercise. Therefore, the best way to treat your spasticity is to attempt to exercise your affected muscles.
Even imagining movements, but especially activating your muscles will reinforce new neural pathways. The goal is to improve the communication between your brain and muscles and, eventually, lessen spasticity.
But what if your spasticity is so severe you cannot even move your muscles at all? Fortunately, there are alternative treatments for you to try.
Treating Severe Spasticity After TBI

Spasticity can resolve on its own as the brain heals. But in some cases, spasticity is so severe that the opposing muscle groups are unable to overcome the spastic ones This can make engaging neuroplasticity much more difficult.
However, there are therapeutic treatments to consider – here are two common options.
Stretching and Passive Range-of-Motion
Stretching and passive range of motion exercises can help minimize the effects of spasticity after TBI. Stretches are important for preventing contractures, which preserves joint mobility. Keeping muscles limber also prepares the joint for even the weakest movement attempts.
Passive exercises come with an additional benefit though, in that they can also activate neuroplasticity. In fact, neuroimaging studies have found that passive movement exercises activate the primary motor cortex, the part of the brain responsible for voluntary movement.
Therefore, having a therapist or a family member move your arm or leg for you can help repair the brain’s connection to controlling your muscles. And the stronger the communication, the less spasticity you will experience.
Botox Injections and Baclofen Pumps

For patients with spasticity in a single location, Botox injections can prove useful. Botox is a nerve blocking agent that prevents the release of acetylcholine, a neurotransmitter that causes your muscles to contract.
This medication can almost instantly stop painful spasms, which makes it a popular treatment choice for more serious cases. For people with severe and painful spasticity, it is a good option.
If, on the other hand, your spasticity affects many body parts at once, a baclofen pump will probably prove to be more effective. A baclofen pump refers to a small, hockey-puck-sized device implanted beneath the skin. The device then releases small amounts of baclofen into the space surrounding the spinal cord. This allows the medication to impact multiple muscle groups at once.
However, both baclofen and Botox are only temporary solutions. Once their effects wear off, the spasticity will return. For the most effective approach, patients should combine these medications with passive range of motion exercises or active exercise when possible. This is the only way to engage the brain and stimulate neuroplasticity.
Understanding Spasticity After TBI
Spasticity after TBI can be a painful condition. However, it is treatable.
If your spasticity does not allow you to move on your own, consider combining passive range-of-motion exercises with medication. Although you are not moving yourself, the passive exercise still engages plasticity within the brain. This will help repair the neural connections between the brain and muscles.
As communication improves within the central nervous system, your spasticity should decrease. With enough persistence, you can hopefully train your muscles to relax again.