Involuntary body functions like heart rate are regulated by the autonomic nervous system. When a spinal cord injury damages the nervous system, it can cause complications such as tachycardia, which involves an above-normal resting heart rate.
While tachycardia is not very common among spinal cord injury survivors, it’s potentially life-saving to be aware of the symptoms so that you can help someone seek appropriate medical treatment. This article will teach you everything you need to know about spinal cord injury and tachycardia.
Symptoms of Tachycardia
Tachycardia involves a resting heart rate over 100 beats per minute, which is above normal. If you’re experiencing tachycardia after spinal cord injury, it’s crucial to speak to your doctor immediately or seek emergency medical attention. Unmanaged tachycardia puts stress on the heart and increases the chance of life-threatening medical events such as a stroke or heart failure.
Symptoms of tachycardia that every spinal cord injury survivor and caregiver should know include:
- Dizziness
- Lightheadedness
- Anxiety
- Headache
- Tightness in the chest
- Shortness of breath
- Fainting
Your doctor can recommend the best treatment should you ever need urgent medical attention for tachycardia. While the best treatment will vary from person to person, the ultimate goal is to slow down the resting heart rate and get it back to a normal rhythm.
All caregivers who interact with individuals with spinal cord injuries should be aware of tachycardia (and other potential complications of spinal cord injury) and know the symptoms.
To understand the cause of tachycardia after spinal cord injury, let’s look at how the autonomic nervous system works and how an injury to the spinal cord can affect it.
Causes of Tachycardia After Spinal Cord Injury
The autonomic nervous system sends messages throughout the brain, spinal cord, and body to regulate functions such as heart rate, respiration rate, digestion, and more.
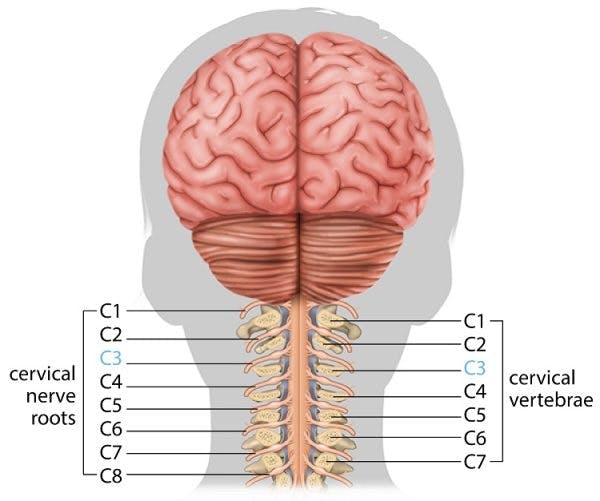
Just like specific areas of the brain control different functions, specific segments of the spinal cord control different functions too.
In regards to spinal cord injury and tachycardia, we’re interested in the T1-T5 levels of the thoracic spinal cord (the upper back area). These segments control heart rate (among many other things).
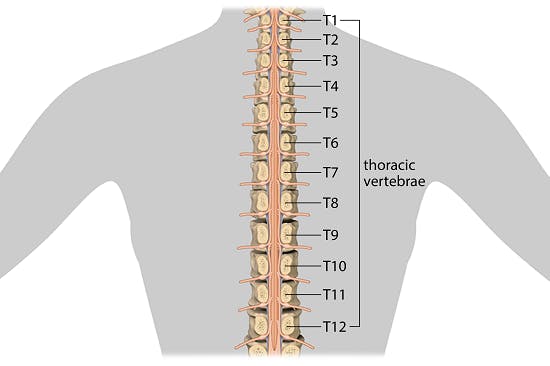
After a spinal cord injury, the connections in the spinal cord become disrupted; and as a result, areas below the level of injury may no longer effectively send or receive communication from the brain. Therefore, a spinal cord injury at or above the sixth thoracic vertebra (T6) can impact heart rate.
In other words, because the T1-T5 segments of the spinal cord control heart rate, individuals with cervical or high-thoracic spinal cord injury may sustain cardiac dysfunctions such as tachycardia, where the resting heart rate is over 100 beats per minute. (Average heart rate is 60-100 beats per minute.)
While tachycardia is more common in people with spinal cord injury levels T6 and higher; tachycardia itself is rare after a spinal cord injury. Instead, the more-common cardiac dysfunction is bradycardia, which involves a resting heart rate below 60 beats per minute.
Bradycardia vs Tachycardia After Spinal Cord Injury
The link between bradycardia (slow resting heart rate), tachycardia (fast resting heart rate), and spinal cord injury involves both the sympathetic and parasympathetic nervous systems. These branches of the autonomic nervous system work synergistically by counteracting each other.
- Sympathetic nervous system: This is your fight-or-flight response. When activated, it increases functions like heart rate, alertness, and blood pressure.
- Parasympathetic nervous system: This is your rest-and-digest response. When activated, it slows down your heart rate, stimulates digestion, and relaxes the blood vessels.
When a spinal cord injury damages the sympathetic nervous system, the individual may experience neurogenic shock. During neurogenic shock, the damage to the sympathetic nervous system results in unopposed parasympathetic stimulation. In other words, the body’s relaxation response takes over without restraint. When this happens, the fight-or-flight response cannot oppose the rest-and-digest response.
For individuals with cervical or high-thoracic spinal cord injuries, resting heart rate may slow down because of an overpowering parasympathetic response, potentially resulting in bradycardia. This is what makes tachycardia less common.
Tachycardia as a Secondary Effect
Because tachycardia is rare, it’s worth looking into two more conditions that may contribute to tachycardia after spinal cord injury: 1) autonomic dysreflexia and 2) complications when treating bradycardia.
When Autonomic Dysreflexia Contributes to Tachycardia
Autonomic dysreflexia, a potential complication of spinal cord injury, describes a reflex action that causes the autonomic nervous system to overreact when it encounters a potentially damaging (noxious) stimulus below your level of injury.
Normally, a noxious stimulus like touching a hot stove triggers the fight-or-flight response to reflexively move away from the hot surface. After a spinal cord injury, however, the message of pain or irritation may not reach the brain appropriately and the body may enter this reflexive, heightened state for a prolonged period of time.
Of the many symptoms of autonomic dysreflexia, tachycardia is one of them. Furthermore, autonomic dysreflexia occurs in about half of individuals with spinal cord injuries at the T6 level and higher, which is the same population at risk of tachycardia. Therefore, spinal cord injury survivors can help manage tachycardia by carefully avoiding triggers for autonomic dysreflexia such as a full bladder.
Learn more about the triggers for autonomic dyreflexia »
Tachycardia as a Complication When Trying to Treat Bradycardia
Sometimes treatment for bradycardia (lower-than-normal resting heart rate) can “overcorrect” for the condition and cause tachycardia (higher-than-normal resting heart rate) as a complication. Bradycardia treatment, which may involve medication, focuses on increasing heart rate. When the dose of treatment is too high or the body acts adversely to it, resting heart rate may increase too much and cause tachycardia.
For this reason, it’s important for all spinal cord injury survivors and caregivers to be aware of the symptoms of tachycardia, even if they are being treated for bradycardia.
Understanding Tachycardia After Spinal Cord Injury
Tachycardia occurs when resting heart rate rises above 100 beats per minute. When it remains in this above-normal state, the heart is put under potentially-fatal stress.
While tachycardia is rare after a spinal cord injury, it can be a complication of autonomic dysreflexia, which occurs in almost half of individuals with cervical and high-thoracic spinal cord injuries. Because of this risk, survivors should learn about autonomic dysreflexia and take great care to avoid triggering it.
As you can see, attention and awareness can help save a life. We hope this guide has helped you better understand spinal cord injury and tachycardia.