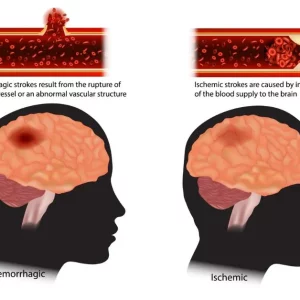
A stroke in the motor cortex can cause difficulties with muscle activation, functional movement, and coordination. This is because the motor cortex houses your brain’s movement center, which is responsible for activating muscles to perform different tasks. As a result, stroke survivors with damage to the motor cortex may experience movement impairments that can make activities of daily living difficult.
Fortunately, because of the brain’s ability to heal and create new pathways, it is often possible to improve these impairments. Through time and consistency with rehab, some survivors can even reverse many of the effects of a motor cortex stroke.
Following a stroke in the motor cortex, the different aspects of recovery can feel overwhelming. To help you navigate this complex time, this article will help you understand more about how the motor cortex functions. Then we will talk about what a stroke in this area of the brain can entail. Additionally, we will discuss your brain’s natural repair mechanism and different treatments available after a motor cortex stroke.
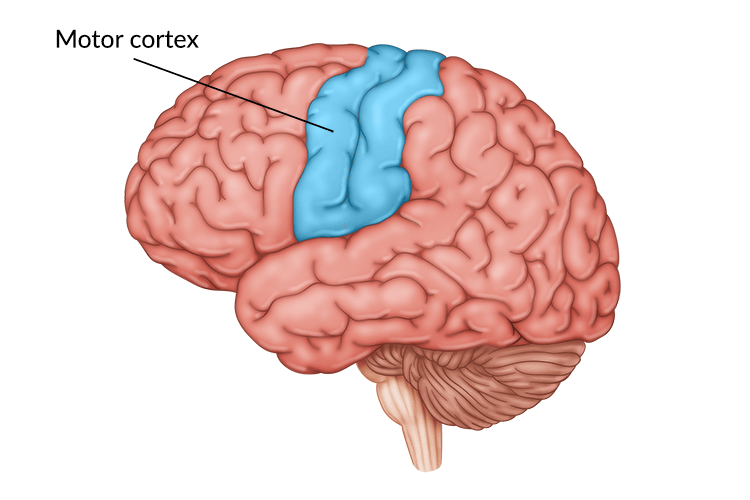
What is the Motor Cortex?
The motor cortex is an area of brain tissue located in the frontal lobe, sitting just in front of the parietal lobe. The motor cortex can be further divided into three different sections with slightly different functions. These three sections that comprise the motor cortex are the:
- Primary motor cortex
- Premotor cortex
- Supplementary motor area
These three areas are responsible for initiating and coordinating voluntary movements. Voluntary movements are movements that are purposeful or intentional. This can include everything from moving your hands and legs to controlling facial expressions and even performing some swallowing motions.
The primary motor cortex is responsible for creating the signals necessary to initiate these voluntary movements. These signals then cross over the body’s midline to activate muscles on the opposite side of the body. This means that the movements on the right side of your body are controlled by the left hemisphere of the primary motor cortex, and vice versa. Therefore, if a stroke occurs in the left hemisphere, you will see the effects on your right side.
How the Motor Cortex Works
The different sections of the motor cortex control different aspects of movement. For example, the premotor cortex is responsible for planning movement, and the primary motor cortex initiates the execution of that movement. Additionally, the primary motor cortex helps determine the force of the movement as well as that movement’s direction.
The primary motor cortex is arranged in such a way that different parts of the cortex control different parts of the body. However, not every part has equal amounts of brain matter devoted to it. This organization of the motor cortex is mapped out by something called the motor homunculus. Complex movements that require more precise control take up larger amounts of space in the brain than simple motions do.
To give you an example, a significant portion of the motor cortex is devoted to finger movements and facial expressions. This is because so much motor control is needed to perform the small, intricate motions of the fingers and the face. In comparison, a smaller portion of the brain is responsible for leg motions since these movements are larger and require less precision.
This fact explains why many stroke patients struggle with fine motor control or facial paralysis. Since those motions are controlled by a larger portion of the motor cortex, they may have a higher likelihood of becoming impaired during a stroke.
Effects of Stroke in the Motor Cortex
A stroke in the motor cortex can cause a variety of physical effects, some being more serious than others. As we discussed previously, this depends largely on the area of the motor cortex most affected and the size of the stroke. Some common secondary effects of motor cortex damage include:
- Hemiparesis. This refers to weakness on one side of the body. If a stroke has damaged the left motor cortex, the patient may have trouble lifting their right arm, moving the fingers on their right hand, or controlling their right leg movements. Additionally, the right side of their face might droop. Hemiparesis can also affect trunk movements, so patients with this condition may have trouble balancing due to weakness in their core muscles on the affected side.
- Hemiplegia. Hemiplegia is more severe than hemiparesis as it refers to paralysis of one side of the body. This can have a major impact on a survivor’s mobility and independence. Additionally, prolonged immobility sometimes contributes to edema, or swollen limbs.
- Spasticity. Spasticity occurs after a loss or disruption of communication between the brain and muscles. When spasticity occurs, the muscles are in a constant state of contraction or spasm. If this situation persists, the muscle fibers can shorten and lead to contractures.
- Loss of fine motor skills. The ability to perform the small, intricate movements of the hands and fingers is referred to as fine motor skills. When a stroke occurs in the motor cortex, the survivor may lose the ability to perform these small movements of the hands, fingers, and wrists. This makes activities of daily living such as eating, bathing, and dressing difficult.
- Speech and swallowing problems. The motor cortex controls many of the muscles used during speech. Therefore, if a stroke damages this area, speech difficulties can occur. This can include various forms of aphasia. Additionally, difficulty swallowing (dysphagia) can also result from weakness of the muscles of the mouth and throat.
- Incontinence. A stroke in the motor cortex can weaken and reduce coordination of the muscles that control bowel and bladder functions. This effect usually occurs immediately after stroke but typically improves after the brain has had time to heal.
- Upper motor neuron syndrome. This syndrome refers to a collection of symptoms that can sometimes be seen after tissue damage in and around the motor cortex. This includes effects like muscle weakness, spasticity, clonus (involuntary muscle contractions), and abnormal reflexes.
As you can see, stroke in the motor cortex can lead to a wide range of symptoms, such as the ones we discussed above. The specific type of symptoms you experience will depend on the precise location of the stroke. Fortunately, you can treat these effects through rehabilitation that includes physical, occupational, and speech therapy. To help you get started, we will discuss how these treatments work in the next section.
Stroke Rehabilitation through Neuroplasticity
When a stroke causes damage to brain tissue, some of these areas will lose their function. However, it is still possible to regain lost functions after stroke by rewiring these functions to other, unaffected areas. This can take place because the brain possesses a remarkable healing ability known as neuroplasticity.
Neuroplasticity allows the brain to reorganize neurons and compensate for damaged areas of brain tissue. This strengthening and rewiring of neural pathways is the basic principle behind many therapy protocols. This is because neuroplasticity is encouraged through the high repetition of therapy exercises, sometimes called massed practice.
At the beginning of stroke recovery, your therapy team will help you practice activating specific muscle groups, such as the muscles of the hand. This will require significant effort and concentration at first because the brain will be establishing new neural pathways. Fortunately, the more you practice that movement, the more you will reinforce those pathways.
With time, these new pathways can become more established and the movements will become easier to perform. For this reason, the best way to improve function after a stroke in the motor cortex is to engage neuroplasticity through consistent exercise.
Why Early Intervention Is Crucial
During the first three to six months after stroke, the brain enters a heightened state of plasticity. We call this period when the brain makes rapid, meaningful gains in function spontaneous recovery. This means therapy will have a more visible impact and patients can make faster progress toward their goals during this time.
Therefore, it is crucial to begin rehabilitation including physical, occupational, and speech therapy as soon as possible after a stroke in the motor cortex. This allows patients to take advantage of their heightened plasticity. Additionally, these therapists can recommend appropriate adaptive equipment to help survivors and caregivers improve the performance of daily care tasks.
After discharge from the hospital or inpatient rehab, stroke patients should continue to practice home therapy exercises as much as possible, especially in the early days of recovery. The more consistently you activate neuroplasticity, the more progress you will make, even if this progress is slow. Many survivors experience plateaus in progress or even occasional regressions after stroke. Thankfully, we know it is possible to continue recovering long after your stroke took place.
Your therapists may recommend going to outpatient therapy in addition to participating in a home exercise regimen to ensure the best results. We know that staying consistent with a home program can be difficult, so it is important to work closely with your rehab team to create a program that is unique to your goals.
Rehabilitation technology like Flint Rehab’s FitMi home therapy is attractive for patients recovering from this type of stroke because it encourages high repetition of therapeutic exercises. This can help you stay motivated and consistent with your program to keep taking steps toward recovery.
Recovering from Stroke in the Motor Cortex
A stroke in the motor cortex can result in a large variety of motor symptoms. This is because this area of the brain is responsible for coding the signals needed to tell your body to move. As a result, survivors often experience secondary effects such as weakness, paralysis, spasticity, and difficulty with speech or swallowing.
The effects of this type of stroke are serious and can lead to major changes in daily life for a survivor. However, you can recover many affected motor functions by activating neuroplasticity through repetitive exercise. With enough practice, you can help your brain rewire itself until you regain the strength to move your body more freely and independently.
We hope this article has helped explain the effects of stroke in the motor cortex as well as the recovery process. Continue practicing your rehab exercises consistently and seek support from those around you. There is always hope for recovery, even years after your stroke.