A thalamic stroke can have unique effects for every survivor. To understand how a stroke in the thalamus affects the body, it helps to learn what happens when a stroke occurs and which functions the thalamus controls. This article will explain just that, along with an overview of the recovery process.
Use the links below to jump straight to any section:
Understanding a Stroke in the Thalamus
A stroke occurs when the supply of blood to the brain is compromised. This can happen when an artery leading to or within the brain becomes clogged by a blood clot (known as an ischemic stroke) or when a blood vessel bursts (known as a hemorrhagic stroke).
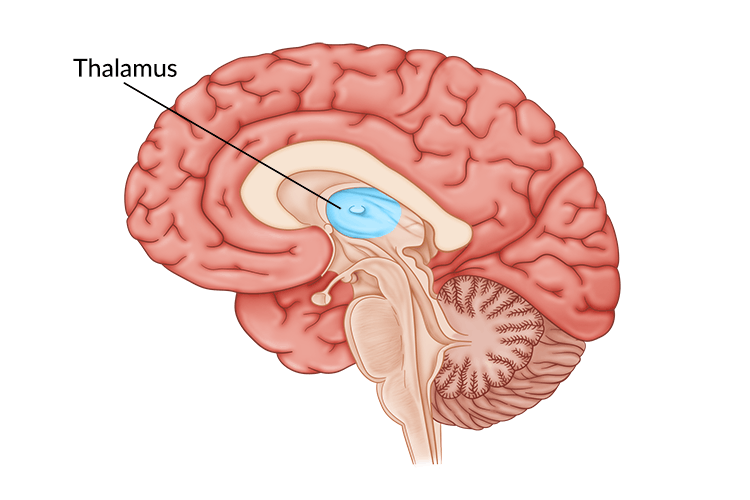
A thalamic stroke occurs when a blocked or ruptured artery disrupts blood flow to the thalamic area. The thalamus is located nearly in the center of the brain, directly between the two hemispheres. Therefore, thalamic strokes fall under the category of subcortical or lacunar strokes, which affect the deeper brain regions beneath the outer cerebral cortex.
When a stroke occurs, it is a medical emergency because brain cells begin to die within minutes of losing blood supply. As a result, restoring blood flow as quickly as possible is crucial to saving the person’s life.
Survivors of stroke that receive swift treatment usually experience fewer secondary effects and functional impairments than those who receive delayed treatment. Rehabilitation should begin as soon as possible after medical treatment for a stroke to address any resulting secondary effects.
Understanding the Effects of a Thalamic Stroke
Each area of the brain controls different functions. Depending on where a stroke occurs, a number of physical, cognitive or psychological functions may be affected. A thalamic stroke can impair the functions typically controlled by the thalamus. Therefore, looking at the typical role of the thalamus can provide insight into the possible secondary effects of a thalamic stroke.
The thalamus plays a key role in many functions, including memory, emotions, the sleep-wake cycle, executive functions, sensory processing, and motor control. Often called the brain’s relay center, it is responsible for relaying 98% of all sensory input throughout the body.
In fact, each sensory system, with the exception of the olfactory system (sense of smell), has a specific part of the thalamus designated to relay its information to the outer parts of the brain for processing. Therefore, problems related to the senses after a thalamic stroke are common.
Potential secondary effects of a thalamic stroke include:
- Impaired sensation. Numbness or tingling sensations are common after a thalamic stroke.
- Sleep disturbances. Individuals may struggle with insomnia or excessive daytime sleepiness after a stroke in the thalamus.
- Amnesia. A thalamic stroke may result in memory loss (vascular thalamic amnesia) that can affect long- or short-term memory. It can also be accompanied by a shift in personality.
- Changes in attention. Attention, along with memory, is a high-level cognitive skill that the thalamus plays a role in. Thus, a stroke in the thalamus can affect an individual’s ability to pay attention.
- Speech difficulties. Language and communication difficulties such as aphasia may occur after a thalamic stroke.
- Hemispatial neglect. This causes the individual to be unaware of their environment on the side of the body opposite the damaged area of the brain. It usually occurs when the right hemisphere of the brain is affected, leading to neglect of the opposite side of the body (left neglect).
- Vision impairments. There are many types of vision impairments that can occur after a thalamic stroke, such as diplopia (double vision) or hemianopia (loss of half of the visual field).
- Difficulties with balance. The brain stem, which is near the thalamus, helps regulate vertical eye position and head posture. When these functions are affected by a stroke, it can result in poor balance, which can also cause walking challenges.
- Central post-stroke pain. This involves chronic neuropathic pain, also known as thalamic pain when following a thalamic stroke.
Thalamic Pain Syndrome
Thalamic pain is a relatively common secondary effect after stroke, affecting up to 8% of survivors. Furthermore, thalamic pain syndrome is a chronic condition that can have delayed onset, taking months or even years after a thalamic stroke for pain to develop..
While thalamic pain may initially present as impaired sensation on the side of the body opposite the stroke. It may later progress into thermal dysregulation, such as freezing or burning sensations, before becoming severe, chronic pain.
Due to its delayed onset, thalamic pain may be especially difficult to diagnose. This makes it essential to communicate with one’s medical team regarding any concerns following a stroke.
The Recovery Process After a Thalamic Stroke
Recovery from a thalamic stroke focuses on restoring and compensating for the abilities compromised by the stroke. While not all secondary effects can be resolved, the intensity and timeliness of rehabilitation has a meaningful impact on how much function one can recover.
Pursuing intensive rehabilitation early on and making an effort to integrate skills learned during rehabilitation into one’s daily life can optimize recovery outcomes. The following are some treatment techniques that thalamic stroke survivors may use during their recovery process:
1. Physical Therapy
When a thalamic stroke leads to motor impairments, physical therapy can help restore movement in the body. Common goals for physical therapy include improving gait (manner of walking), posture, balance, and strength. If needed, physical therapists are also able to recommend and train individuals to use the appropriate type of walker or cane to move around safely.
Want 25 pages of stroke recovery exercises in a PDF? Click here to download our free Stroke Rehab Exercise ebook now (link opens a pop up for uninterrupted reading)
2. Occupational Therapy
Occupational therapy for stroke can also help survivors regain mobility, particularly related to the activities of daily living such as eating and dressing. Therapists can also recommend and provide education regarding adaptive equipment and compensation techniques to help minimize difficulties with daily tasks, such as using a grab bar or shower chair for those with poor balance.
3. Sensory Reeducation
After a thalamic stroke, it’s common for survivors to experience sensory issues such as numbness, tingling, pins-and-needles sensations, or pain. Often introduced by an occupational therapist, sensory retraining is a technique involving various exercises to stimulate the tactile sensory system. This can encourage the brain to adapt and improve its ability to interpret sensation accurately.
For example, one sensory retraining exercise may involve alternating between placing hot and cold towels on the arms to stimulate the brain’s ability to process different temperatures. Another exercise could involve rubbing objects of various textures along the affected areas of the body.
While sensory retraining can be an effective technique for those experiencing sensation impairments, it is important to use caution. Since the brain is unable to process sensations accurately, objects that may not feel too hot, cold, or painful to an affected area of the body could cause damage over time. Always talk with a therapist before using sensory retraining methods, especially when involving stimulation that could possibly be harmful.
4. Vision Therapy
Vision rehabilitation therapy may consist of eye exercises and/or compensation techniques to help those with visual impairments regain their vision. Not all survivors respond to this therapy, but some are able to achieve partial or full vision recovery.
Depending on the type of visual impairment, eye exercises may be used to retrain the brain how to control the eye muscles. Different techniques to compensate for visual field deficits or inattention may also be introduced. For example, many individuals benefit from using the lighthouse strategy, which focuses on visually scanning side to side like a lighthouse light to see an entire area.
5. Speech and Cognitive Therapy
Thalamic stroke survivors may experience secondary effects such as speech difficulties and changes in executive function. Executive function refers to higher level cognitive functions, such as working memory, attention, and judgement. A speech-language pathologist (SLP) can address both communication and cognitive changes following thalamic stroke through targeted exercises and compensatory techniques.
For example, an SLP may use speech therapy exercises focused on tongue and lip movements to help with those having trouble with producing specific sounds. Cognitive exercises and strategies such as remembering a short list of groceries or using a planner to keep track of appointments can also be used to help survivors improve executive functioning skills.
6. Pain Management
Seeking treatment is critical for survivors with central post-stroke pain. Some stroke survivors may find relief through medication or alternative medicine. When nonsurgical pain treatment options fail to provide relief, survivors should consider talking with their doctor about surgical options such as a permanent spinal cord stimulator implant.
Seeking both social support and medical treatment is crucial for overall health and wellbeing. Chronic pain support groups can be an excellent way for individuals to express their challenges, learn from others’ experiences and combat the psychosocial effects of living with chronic pain.
Appropriate treatment techniques vary depending on which secondary effects of thalamic stroke survivors experience. For an optimal recovery, it is best to pursue recommended interventions as soon as possible.
Optimizing Recovery Outcomes
Since the secondary effects of thalamic stroke are caused by damage to the brain, it is essential to address this damage in order to recover. The brain has the amazing ability to rewire itself to allow healthy areas of the brain to take on functions previously controlled by the damaged areas. This occurs through a process called neuroplasticity.
Consistent and repetitive practice of tasks involving affected functions is the best way to stimulate neuroplasticity. Pursuing therapy soon after a stroke is also very beneficial, as the brain enters a heightened state of neuroplasticity during the first few weeks and months after the incident. Since the brain is more adaptable at this time, individuals are likely to recover functions more quickly and effectively.
Therefore, one of the best ways to achieve an optimal recovery is to continue practicing the skills and exercises learned in therapy at home. This allows the brain to continue being stimulated on a regular basis, rather than just during therapy sessions. While it is possible to recover without using specialized home therapy equipment, many home-based neurorehabilitation devices have been developed to improve survivors’ recovery outcomes.
For example, Flint Rehab’s FitMi home therapy helps turn classic rehab exercises into a gamified, interactive experience adjusted specifically to the survivor’s skill level. Similarly, the CT Speech & Cognitive Therapy App focuses on improving cognition and communication by providing an assessment and recommending exercises based on the survivor’s ability level.
By using neurorehabilitation devices at home, individuals are more motivated to continue working toward their recovery, and are likely to have more optimal results. Consistently practicing tasks involving affected functions is key to recovery following a thalamic stroke.
Recovering from a Stroke in the Thalamus
A thalamic stroke can result in a variety of secondary effects, including sensation changes, cognitive problems, and thalamic pain. The best treatments for thalamic stroke vary depending on which functions have been affected. Many individuals pursue physical, occupational and/or speech therapies as well as pain management interventions in order to achieve an optimal recovery.
Recovery from a thalamic stroke involves hard work, dedication, and consistency. Repetitive practice, both during and outside of therapy, stimulates adaptive changes in the brain. With consistent practice, survivors have hope for recovery following a thalamic stroke.