For those living with the dual effects of traumatic brain injury and PTSD, the combination can be overpowering.
PTSD cannot only severely impact a person’s mental and emotional health, but it also makes it much harder to take the right approach to traumatic brain injury rehabilitation.
This is why it’s so important to address any signs of PTSD early on in your recovery. However, it’s sometimes hard to differentiate the symptoms of TBI from PTSD, because the two often feed off each other.
In this article, we’ll cover some of the defining characteristics of PTSD after a brain injury and show you the best ways to treat it.
Relationship Between Traumatic Brain Injury and PTSD
PTSD refers to a mental health condition that arises following exposure to significantly traumatic events such as combat, assault, or near-death experiences.
Traumatic brain injury refers to damage to the brain caused by an outside force, usually a violent blow or blast.
In the past, most doctors believed that PTSD could not occur after a brain injury, because most TBI survivors had no memory of the traumatic event. Today, however, research strongly indicates that PTSD can indeed occur after a traumatic brain injury.
In fact, PTSD is almost three times more likely to develop after a TBI than after other types of injuries. For example, in a recent study, 43% of soldiers who suffered a blast-induced TBI met the criteria for PTSD. In contrast, only 16% of soldiers with other bodily injuries met the criteria for PTSD.
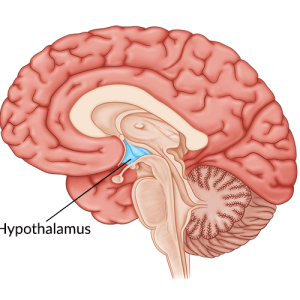
The precise reason that PTSD occurs after brain injury is still unclear, but it may be caused by a change in the parts of the brain that process trauma. After a traumatic event such as a brain injury, the brain releases adrenaline and other hormones to give the body a burst of energy. This usually fades once the danger passes.
With PTSD however, the brain remains “stuck” in a prolonged heightened state of alert. This heightened state causes many of the symptoms associated with PTSD.
Diagnosing PTSD Symptoms After Traumatic Brain Injury
PTSD and traumatic brain injury share many characteristics. Unfortunately, this can make determining the origin of a person’s symptoms quite difficult. Some common symptoms the two share include headaches, light and noise sensitivity, difficulty concentrating, anxiety, and insomnia, among other side effects.
However there are a few symptoms that are more unique and indicative of PTSD. These include:
- Involuntary recurring thoughts of the life-threatening event
- Avoiding people and places that remind you of your injury
- Emotional numbness and feeling detached from friends and family
- Overwhelming feelings of shame and guilt
- Hypervigilance, i.e. constantly feeling on your guard, irritable, or easily startled
- Angry outbursts or aggressive behavior
While some of these symptoms can also overlap with TBI (especially irritability and angry/aggressive outbursts), what distinguishes PTSD from ordinary brain injury symptoms is feeling immobilized by them.
In other words, you can’t ignore these feelings, they are interfering with your daily life, and you are unable to move forward. You feel stuck, like your feet are sinking in quicksand. That is PTSD.
Additionally, the symptoms of PTSD can last for months or years. While some remaining deficits from TBI can last a long time as well, the intensity of the emotional and behavioral symptoms should begin to fade after a few months.
Treating Traumatic Brain Injury and PTSD

Treating traumatic brain injury and PTSD can be a complicated process and requires the oversight of a trained neuropsychologist.
One reason it is difficult to treat PTSD after brain injury is because many traditional PTSD medications can be harmful to people with TBIs. For example, the tranquilizing drugs that doctors often prescribe to PTSD patients could be dangerous if you have suffered a brain injury.
That’s because, after a brain injury, we want to avoid suppressing any more cognitive functions. This explains why it is critical to know whether someone’s symptoms stem from their traumatic brain injury or PTSD.
Although there have been groundbreaking studies that show that brain scans can accurately distinguish between PTSD and traumatic brain injury, it might be some time before those scans are widely available to the public.
In the meantime, treatment for PTSD after TBI should focus on techniques that won’t cause further harm to the damaged brain. The following are a few examples of treatments that can be effective at treating the symptoms of both TBI and PTSD:
1. Talk Therapy

Talking about your injury with someone can help you learn coping skills to find relief from your negative symptoms.
Sometimes antidepressant medications used together with traditional psychotherapy is very effective for overcoming PTSD after brain injury.
However, make sure you consult a doctor familiar with your injury before you start a medication. It’s important not to take something that suppresses brain activity since that will only worsen your other TBI symptoms.
2. Cognitive Behavioral Therapy (CBT)
Cognitive-behavioral therapy is a more intensive form of psychotherapy that focuses on identifying harmful thoughts and beliefs which trigger negative feelings.
Cognitive-behavioral therapy is based on three core principles:
- Beliefs create feelings
- Feelings dictate behavior
- Behavior reinforces beliefs
Therefore, to get to the root of PTSD, most CBT treatments focus on uncovering unhealthy thinking patterns. Once you identify these thoughts, a therapist will help you essentially rewire your thoughts to trigger good feelings instead.
It is a safe and effective intervention for people suffering the effects of traumatic brain injury and PTSD.
3. Meditation

Mindfulness and meditation techniques can be effective ways to calm the overstimulated mind. It can also help treat PTSD after traumatic brain injury.
Mindfulness simply refers to the practice of focusing on the present and cultivating awareness of your surroundings. It means keeping your attention on what is happening right now and not on the future or the past. This makes it an excellent antidote to PTSD, which often forces patients to relive their most painful memories.
In fact, studies indicate that certain meditation techniques such as Mindfulness-Based Stress Reduction significantly reduced symptoms in PTSD patients.
It might feel odd at first, especially if you’ve done nothing like it before, but it’s worth trying and seeing if it helps with your symptoms.
PTSD and Traumatic Brain Injury
PTSD is a debilitating condition, with or without a traumatic brain injury. But it doesn’t have to be the end of your story, and it doesn’t have to consume you.
In fact, many TBI patients, by using the techniques above, have found effective ways to overcome their PTSD. As a result, they discovered a strength inside them they never knew existed.
With the right combination of treatments, you also can overcome post-traumatic stress disorder and find strength and peace again after your injury.